Posted on: 12 April 2019
Hello, my name is Richard...
Kia Ora!
How to respond to the horrors of this day? With kindness. A hello. A nod. A word. We’re a family of many faces and cultures and houses. A mosque is my house. A synagogue is my house. A temple is my house. A Marae is my house. We are a family and families look after each other.
That’s a quote from a New Zealander Nigel Latta on Twitter (@NigelLatta) in response to the recent terrorist murders in Christchurch.
I’m writing this blog a stone’s throw away from Christ Church in Harrogate, with Christchurch, Canterbury, New Zealand on my mind.
I’ve just returned. Personal trip, holiday, funded by me - and with a bit of work thrown into the mix.
Just thinking back to Friday 15th March. 7am WhatsApp from friends in Rotorua: “there’s been a shooting in Christchurch”. Understatement. An extremist gunman had been on a killing spree at two mosques, with at least 50 people dead and many more injured.

We had just spent a week living and working in the city, staying in a house in the suburb of Merivale, which is separated from the city centre by Hagley Park – for those of you who know Newcastle, think Gosforth and Jesmond, across the Town Moor.
 We were less than a mile from Deans Avenue Mosque, where at least 41 people died on that Friday lunchtime. I ran so near it, around Hagley Park, zigzagging across Riccarton Avenue and bordering Deans Avenue. In the evening sunshine, as teams played rugby and football, no city could have felt safer or more harmonious.
We were less than a mile from Deans Avenue Mosque, where at least 41 people died on that Friday lunchtime. I ran so near it, around Hagley Park, zigzagging across Riccarton Avenue and bordering Deans Avenue. In the evening sunshine, as teams played rugby and football, no city could have felt safer or more harmonious.
Awful, tragic, unimaginable. All those words that we all use following a terror outrage. And yet somehow this feels more personal. For Christchurch is a city that gets under your skin. There’s just something about it and its people.
This is not the first time this city, sometimes called the most English of NZ’s cities, has faced tragedy. Cantabrians are still recovering from the major earthquakes in 2010 and 2011.
We had read, and talked to lots of people, about the devastation left by the quakes but nothing quite prepares you for the site of the shattered Victorian Cathedral, gaping roof.
We arrived the day after the 8th anniversary of the February 2011 quake in which 185 people died. If the personal stories at quake story bring you to point of tears, then the serenity of the 185 empty chairs that mark the lives of everyone who died is something else. Each chair is individual. Every type of chair that you can imagine. Wheelchairs. Baby-carriers. Their memory lives on.

In so many conversations, particularly when spending three days shadowing colleagues at Canterbury District Health Board, I heard that people were running on empty; they’d been adrenalin-powered for nearly a decade; post-traumatic stress was an underlying constant; public servants rescuing others were finding themselves in need of emotional rescue. Whilst the city’s essential services and infrastructure were recovered very quickly, many people are still repairing their homes and resolving insurance claims.
In the last three weeks, I’ve messaged people I met and worked with. One manager woman told me that the husband of one of her team had been on his way to the mosque that Friday when his car broke down. He never made it there and this probably saved his life. Another colleague said the next generation are angry: traumatised by quakes and now terror. He hoped that they would stay with the city and told me how health and community services were now planning a massive effort with schools, through their Mana Ake (Maori for “stronger for tomorrow”) programme, to restore hope for the future.
A special newsletter from David Meates, Canterbury Health Board’s Chief Executive captured what people have been feeling and how health and social care services have responded.
And yet, for all of the dark times, Christchurch is a city where new energy stirs. There is a renaissance going on. New buildings, like Turanga, the impressive new city library, and the new acute hospital are springing up all the time. A convention centre is on the way. The Cathedral will be re-built.

 In the gaps, where buildings once stood, there are, literally, Gap Fillers: Street art and community regeneration that provokes, challenges, makes you smile, creates talking points. Check them out, alongside www.watchthisspace.org.nz Where else in the world do you get a giant arcade game across the street? Or a “dance-o-mat” where you put NZ$2 into a washing machine, link up your phone and dance to your chosen playlist for half an hour?
In the gaps, where buildings once stood, there are, literally, Gap Fillers: Street art and community regeneration that provokes, challenges, makes you smile, creates talking points. Check them out, alongside www.watchthisspace.org.nz Where else in the world do you get a giant arcade game across the street? Or a “dance-o-mat” where you put NZ$2 into a washing machine, link up your phone and dance to your chosen playlist for half an hour?
Work-wise, I had read the King’s Fund reports about the Canterbury model and with various North Yorkshire and York colleagues had talked with the architects of that system when they led a workshop in York last autumn.

So, I undertook five working days with Auckland and Canterbury District Health Boards, Wellington City Council and PWC NZ.
At first glance, the NZ system looks similar to health and social care in the UK and yet there are major differences. It was part of a 20th century welfare state model; the building blocks are similar, including partner-led GP practices, general and community hospitals, a network of independent care providers and voluntary sector services. However, there are also significant differences. The NZ system was subjected to greater marketization in the 1980s and 1990s. Most people pay a fee to visit the GP – unless they are under 14 or live in the poorest households. A national quango, the Accident Compensation Corporation, uses a national insurance scheme to fund a large share of emergency, urgent and accident-related care. Personal care at home is free and residential and nursing care is means-tested. It is rare for people to move into a residential or nursing care home without assessment from a multi-disciplinary team and/or authorisation from a consultant geriatrician or a gerontology nurse specialist, even if the person is funding the full cost of their care. Equal pay litigation has led to a major pay increase for care workers, funded by central Government, mitigating some of the labour shortages which social care in the UK faces.
 New Zealand has led the World in the growth of retirement villages, settlements of 50-250 apartments or bungalows, within a defined area, with communal facilities and on-site access to a care home. Think McCarthy and Stone writ large, rather than the UK council and housing association model of extra care and supported housing.
New Zealand has led the World in the growth of retirement villages, settlements of 50-250 apartments or bungalows, within a defined area, with communal facilities and on-site access to a care home. Think McCarthy and Stone writ large, rather than the UK council and housing association model of extra care and supported housing.
Health inequalities are an issue. Whilst life expectancy overall is high, Maori and Pasifika communities have much higher premature mortality and morbidity levels and poorer health outcomes. One programme, the Tamaki Project that I visited in the Auckland suburbs of Panmure and Glen Innes, is doing really inspirational work across health, housing and regeneration to put the community in control of its own health and well-being, with some great co-design.
The NZ health and social system is integrated across health and social care and the organisational form, based on 20 District Health Boards (DHBs) (with primary, community, social care and acute hospital responsibilities) has been in place for nearly two decades. GP practices are mostly federated into Primary Health Organisations (PHOs), which are, in many cases, direct providers of a broader range of community services, too. As the current generation of GP partners retires, primary care, as in the UK, faces workforce and ownership challenges. In Auckland, 40% of practices are now owned by private companies. In Christchurch, there is a move towards creating GP-led companies running groups of practices.
 Councils tend to have different remits to their counterparts in the UK. Roles around economic and land planning, arts and culture, leisure, waste and environmental services are similar. However, national ministries and arms-length bodies run policing, social housing, education and children’s social care.
Councils tend to have different remits to their counterparts in the UK. Roles around economic and land planning, arts and culture, leisure, waste and environmental services are similar. However, national ministries and arms-length bodies run policing, social housing, education and children’s social care.
Arguably, cross-sector working is less well-developed than in parts of the UK, although DHBs in Auckland and Christchurch are taking a lead in pushing a much more multi-agency prevention agenda.
Compared with our last visit 14 years ago, I sensed a much greater harmony between respective Pakeha (European White settler), Maori and Pasifika New Zealanders and a strong thread of learning and spirituality from Maori culture informing holistic models of health and social care, whether that be about smoking cessation or self-care. The concept of “whanau” – the extended family - is everywhere, conveying a sense of the wider community as a family.
The relatively new, labour-led, coalition is in policy review mode. It is anticipated that 20 DHBs may well be reduced to a handful, with PHOs following suit. Already, DHBs in the Greater Auckland area are alliancing and Canterbury and West Coast share a single management team. The national fees system for the care sector is up for grabs. Mental Health is an area of increased concern and attention: a national inquiry is generating public and professional debate, talking about a “once in a generation” opportunity for a greater shift towards prevention and the need to re-discover the “missing middle” – people with mental health needs who are excluded from secondary care services but for whom primary care is often not well equipped and supported to provide a comprehensive response.
And so to the Canterbury system, which serves 600000 people in Christchurch, the surrounding towns and plains, large parts of the Southern Alps and the remote West Coast.
Wow!
Canterbury has been on a 15 year journey which started way before the earthquakes, when system leaders realised that, unless they made radical changes, they would need hundreds of extra hospital beds and thousands of additional health and social care workers.
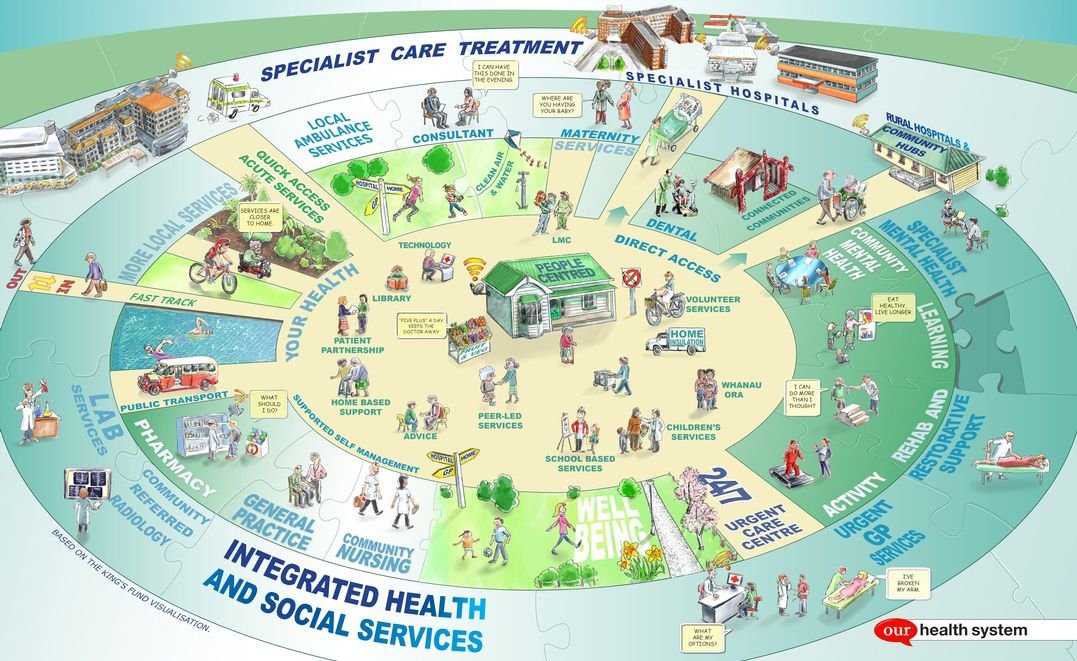
So, they started to build a new model, bringing in a small cross-section of managers and practitioners from across the system to help design it and then paying it forward through similar programmes for hundreds of people, until they had built a social movement. A movement anchored around people’s stories: Agnes, the frail older person, who is pictured in the centre of the diagram below and whose life-sized model house has been re-constructed in a warehouse in a suburban business park.

I spent my first day in Canterbury in that warehouse: the Design Lab.
It’s used for training and service development. Recently they had mocked up part of an entire inpatient ward, so that patients and frontline teams could re-design the ward of the future to ensure privacy, flexible clinical support and hotel-standard views across Hagley Park from each hospital bed.
Key components of the Canterbury model include:
- Aligned budgets across primary, secondary, community and social care
- Systematic adoption of defined protocols for clinical treatment: Health Pathways
- A single leadership team
- Opportunities for clinical leaders to combine clinical, managerial and service transformation roles
- Radical shift of activity to primary care, based around groups of GP practices, with secondary care clinicians working across primary and secondary care – with the assumption that most people’s care will be managed at home and not in hospital
- Integrated health and social care
- Very strong predictive analytics, analysed in real-time by lead managers and clinicians, with a marked shift from performance reporting to pro-active curiosity, debate and action – visting the data ops room is like being on the bridge of the Starship Enterprise!


- A focus on valuing the patient’s time
- 24 hour primary care (including diagnostics, short-stay beds and intensive home treatment)
- A discrete urgent care specialty, which is more developed than the UK equivalent and which bridges the space between primary care and secondary care

The Madras Street centre
Over nearly 10 years, the Canterbury system has:
- Maintained a steady-state in acute hospital bed numbers – against a projection of significant increases
- Reduced non-elective admissions
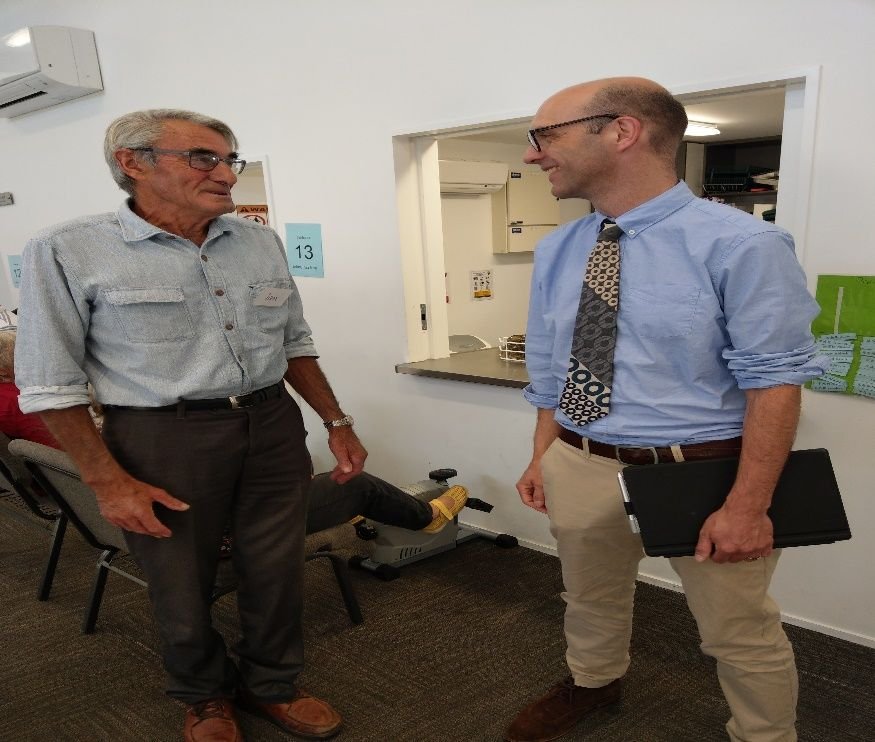 Halved hospital admissions for COPD / respiratory conditions, with a drive to support as many people as possible in primary care – worth reading Dr Mike Epton’s research work on this, including sleep apnoea services, as well as checking out his new project www.wellconnectednz.org and, below, here I am talking to Ian, whose family emigrated from Swaledale, at the pulmonary rehab community exercise programme in Merivale
Halved hospital admissions for COPD / respiratory conditions, with a drive to support as many people as possible in primary care – worth reading Dr Mike Epton’s research work on this, including sleep apnoea services, as well as checking out his new project www.wellconnectednz.org and, below, here I am talking to Ian, whose family emigrated from Swaledale, at the pulmonary rehab community exercise programme in Merivale- Seen significant improvements in falls prevention and consequent sharp reductions in hospital admissions for fractures
- Halved hospital lengths of stay
- Sustained this performance during a period which has included 2 major earthquakes and major disruption to physical infrastructure
Like many parts of the UK health and social care system, Canterbury also faces financial challenges, although a significant proportion of its deficit is due to NZ Ministry of Health re-allocation of funding because of the post-quake infrastructure problems and the perceived de-population of central Christchurch (although in fact, people still remained in the Canterbury DHB area).
Relationships with central Government aren’t necessarily cosy: the Cantabrians’ view of Wellington is akin to the North’s view of London and the feeling is mutual.
For me, it felt like a Sliding Doors counter-narrative: how health and social care could have been in this country if we had built upon the early spirit of PCTs, dodged Shifting the Balance of Power and avoided countless re-organisations. And, perhaps, it is the future we can create for ourselves through our Integrated Care System and a place-based approach to health and social care.
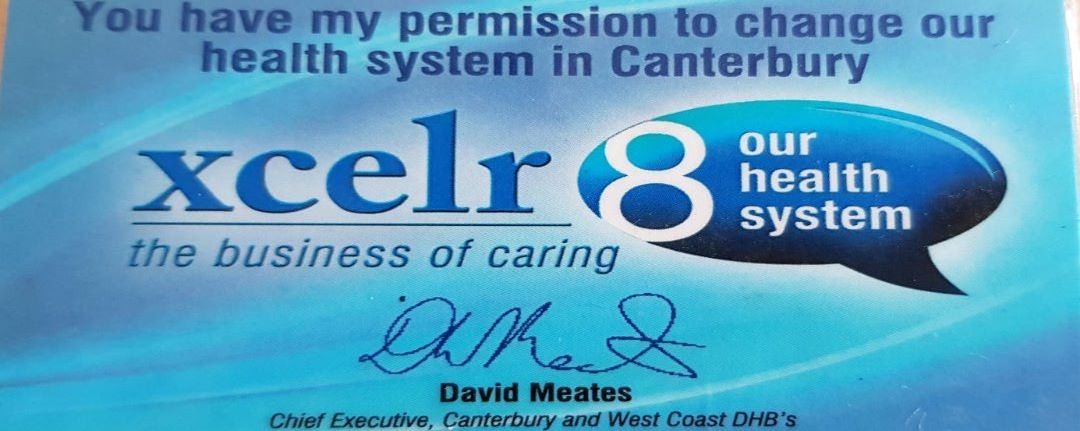
One of the mantras of the Canterbury system is “it’s the people, it’s the people, it’s the people!” And, as always, in creating success, it is the people, the leadership style and the culture which stand out. There’s strong organisational memory – many of the key clinical and managerial leaders have been there from the start. Innovation is encouraged – literally in the form of a ‘permission card’ from the Chief Executive, as well as through re-design programmes. The ethos is one of confidence combined with humility.

And the imprint of the system’s values and priorities was too widespread to be fake or transitory. They really believe it. Doing the right thing and doing things right are the hallmarks of the Canterbury system. In my view, it is even better than the King’s Fund lets on.
And that takes us back to recent events. Whether it is in exemplifying modern compassionate political leadership (The Guardian) or in re-designing health and social care, there is much we can learn from New Zealand.
If you want to help people in Christchurch following the shootings, you can find out more here.
Where there is challenge, there is also hope.
Have a good weekend,
Richard

What else has been happening this week?
Joint Committee Patient and Public Assurance Group
The Patient and Public Assurance Group met on Monday and received an update from Catherine Thompson, Programme Director for the Improving Planned Care Programme, on policies in development such as musculoskeletal and flash glucose monitoring and eye care services (you can read more here). Future developments for the programme include contributing to the Partnership’s response to the NHS Long Term Plan. There was also a presentation on the TV and digital campaign called ‘Don’t be the one’ a campaign which will launch in May about supporting people to stop smoking – you can find out more here. The group also received an update on the ‘Looking out for our neighbours’ campaign and discussed changes in membership to the group due to people moving on to new roles.
West Yorkshire Joint Health and Overview Scrutiny Committee
The Joint Committee brings together West Yorkshire authorities to provide an overview of the West Yorkshire and Harrogate Health and Care Partnership’s work. You can find out more here. It includes local overview and scrutiny committee chairs from Bradford District and Craven; Calderdale, Kirklees, Leeds and Wakefield.
Members met on Monday in Wakefield where there was a discussion on the West Yorkshire and Harrogate Cancer Alliance, led by Professor Sean Duffy, Cancer Alliance Lead and Clinical Director
Carol Ferguson, Cancer Alliance Programme Director. They gave an update on the activity relating to the identified cancer priority / programme, as part of the overall West Yorkshire and Harrogate Health and Care Partnership.
The West Yorkshire and Harrogate Cancer Alliance is one of nineteen nationally designated structures established by NHS England to drive delivery of the national cancer strategy. There is a long history of working at scale across multiple statutory organisations in cancer, driven primarily by the complexity of cancer pathways. It is the exception rather than rule for someone diagnosed with cancer to receive all their care from a single NHS provider organisation, thus it is crucial for all those involved in diagnosis and care to work together to ensure people receive the best outcomes and experience. Moreover as survival rates improve the care of people living with and beyond their treatment requires a more personalised approach to health and wellbeing support in place, in collaboration with specialised health care providers. You can read the full report here.
There was also a report from NHS England regarding access to dentistry across West Yorkshire.
Primary Care and Community Programme Board
The Primary Care and Community Service Programme Board met on Tuesday. The board welcomed an update and overview of the recent publication on universal personalised care and what this means for West Yorkshire and Harrogate by Ruth Twiggins (Personalised Care Site Lead, NHS England & NHS Improvement). Discussion focused on how to ensure personalised care is embedded in the work of the board, wider system and the opportunities presented with the evolvement of primary care networks.
The board received updates on; primary care networks, workforce, and community service benchmarking work before considering in depth the approach to developing the West Yorkshire and Harrogate Primary Care Strategy in time for 1 June. The strategy will set our vision and our plans for transforming primary care in the future, building on the General Practice Forward View and the NHS Long Term Plan. Although a separate document the Primary Care Strategy will form part of the West Yorkshire and Harrogate Five Year Plan.
West Yorkshire and Harrogate Personalised Care Steering Group
The Personalised Care Programme met on Wednesday with new Clinical Lead for Personalised Care, Dr Andy Withers, doing a great job of chairing the meeting. Andy is also the Chair of West Yorkshire and Harrogate Clinical Forum as well as Clinical Chair of Bradford Districts Clinical Commissioning Group.
Jo Webster, Chief Officer for Wakefield Clinical Commissioning Group is the SRO lead for the work.
Jo challenged the group to think about the priorities of the programme which are all about changing the relationship we have with people, as well as a change in more traditional ways of working by focusing on what’s important to people and adopting a more holistic approach including supported self-management, social prescribing, person centered care planning and more choice with the way we use funds to support people’s health and care needs. Key to this is building personalised networks at a local level with the ambitions of learning and sharing good practice across the area.
West Yorkshire and Harrogate are one of eleven Partnerships (also known as integrated care system) supported by NHS England as Personalised Care Exemplar Programmes. We receive support from Ruth Twiggins, programme lead, to take forward this important agenda.
The next steps include delivering personalised care and support training across Bradford District and Craven; Calderdale, Harrogate, Kirklees, Leeds and Wakefield places and to explore and spread a personalised care approach at a workshop on 14 May. More information on the Universal Personalised Care Model can be found here. You can also watch this short film from the Wakefield ‘Live Well’ programme which demonstrates the positive difference this way of working makes to people lives.
There is also information from the event held in February here. You can also view the event report here.
Support for people with learning disabilities – assessment treatment units (ATUs)
In line with NHS England’s Transforming Care Programmes, colleagues working in learning disability services are looking at how best we can provide and deliver community services, including homes and housing, support and care so people can live the life they chose with the support they need. In order to do this colleagues are working together with three Transforming Care programmes across West Yorkshire and Harrogate with the aim to support people with learning disabilities as close to home as possible and to keep them well and out of hospital.
In West Yorkshire there are three Transforming Care Partnerships. They cover Leeds, Bradford, Calderdale, Kirklees, Wakefield and Barnsley.
If and when somebody does need an admission for specialist hospital care (such as assessment and treatment) colleagues will work to ensure that specialist staff are available and that people are not staying in units any longer than needed.
There are three ATUs in West Yorkshire. These are in Bradford, Leeds and Wakefield. Over the past few months we have been looking at the way in which care is provided across the three ATUs and how as a region we make the best collective use of our services. There are currently 22 specialist hospital beds in West Yorkshire. We need to look at reducing this number of beds, so that we can support people with learning disabilities and acute complex needs/challenging behaviour in their local community.
ATU steering group colleagues are looking at how we can work across organisational and geographical boundaries in relation to assessment, treatment unit services and are engaging with people who are currently living in an ATU, their families/carers and staff and also people with previous lived experience of an assessment and treatment centre and their families/carers.
You can find out more here.
Local placed based planners
Colleagues from Bradford District and Craven; Calderdale, Harrogate, Leeds, Kirklees and Wakefield met on Tuesday to discuss local area priorities and plans.
Ian Holmes, Director for the Partnership chaired the meeting and updated people on the work discussed at the recent leadership day including our vision to improve the involvement of people with learning disabilities more in our work and the outcomes of the system oversight assurance group.
There was an update form Karen Poole, Lead for Maternity Programme, on the proposal for the development of children, young people and families programme. This draft proposal will be discussed with the leadership group for their views.
Children and young people up to 18 years old make up one fifth of the UK’s population. Improving their health and wellbeing is an investment in future generations. The NHS Long Term Plan sets out the need to improve care for children and young people.
There is currently no West Yorkshire and Harrogate programme for children, young people and families (albeit a lot of work is taking place in our local areas and across West Yorkshire and Harrogate priority programmes). There was a discussion on the need to build on current partnership work in line with the establishment of a National Children and Young People’s Transformation Programme.
The proposal will consider scoping work for preconception to 18 years (up 25 for additional needs); identifying challenging issues; what can helpfully be done across the whole of the area; and the need to develop a coordinated approach.
We also need to look at the 1001 days (pre-conception to two years). This is in the local plans. It’s important to note this is all about children, young people and families, for example the impact on adults on children and the role of parents. This work will be based on: best start for all; staying safe and with stability; enjoying, learning and achieving; staying healthy; contributing positively to community and society; experiencing economic and environmental well-being and links to other areas such as children in care. Some mapping and gapping work will take place across the area with all partners to ensure we share good learning and practice.
Public Health England also has a community of improvement and produces some good resources linked to the 1001 days and sharing of good practice. You can also read a Health and Social Care Committee Report here for more information.
There was a discussion around the next steps and the importance of working with all stakeholders, including schools, children and families. It’s important that we build on the strengths across the area and avoid duplication of work. We are also keen to look at needs assessments, ensuring families and young people voices are in our programmes, and learning from one another. All draft proposals will be considered further by the Partnership.
Emm Irving (public health manager for prevention and maternity) also updated colleagues on the improving population health work. The NHS Long Term Plan has preventing ill health and early intervention throughout. Emm described the work she and Sarah Smith (public health registrar) have been doing to refresh the prevention at scale programme to have a wider focus on improving population health including; physical health, mental health outcomes and wellbeing of people, whilst reducing health inequalities within and across a defined population. It includes action to reduce the occurrence of ill-health, such as addressing wider determinants of health, for example unemployment and poverty, and requires working with communities and partner agencies.
Identifying and prioritising opportunities to work collectively at scale whilst taking into account the different levels starting with the person first are key areas. There was also a conversation on establishing appropriate working groups to lead on specific projects with cross cutting themes at scale / system level. Initial working group thoughts include: prevention at scale; health and housing; partnership programmes and health inequalities.
Health inequalities at a West Yorkshire and Harrogate level will be a new approach. A decision has been made to focus on the 10% of most deprived people (around 500,000 people) across our six local areas.
The aim is ensure we add value, incorporate feedback from our local places and partners alongside national strategy. We need to define where West Yorkshire and Harrogate work could add value.
West Yorkshire and Harrogate Priority Programme meeting
West Yorkshire and Harrogate priority programme leads met on Thursday. This included colleagues from cancer, digital, personalised care, primary and community care; capital and estates; improving planned care; preventing ill health; maternity and the Academic Health Science Network.
Carol Ferguson, Programme Director for the Cancer Alliance gave an overview on work with hospital colleagues on cancer waiting time system solutions and attendance at the West Yorkshire and Harrogate Joint Health and Overview and Scrutiny Committee on Monday – where there was a discussion on engagement, lay member representation and end of life care.
Emm Irving gave an update on the work taking place across the maternity programmes (please see above). The Local Maternity System Board is waiting to hear on national funding arrangements.
Sarah Smith (public health registrar) is working with public health colleagues and other council partners on the population health management approach which links to the work of health inequalities. The health inequalities project group meet today to consider the NHS Long Term Plan and how we support people who live in our most deprived areas.
Colleagues from the digital programme will be out and about meeting local GPs over the coming weeks. There is a digital showcase event in June about digital programmes including local health care records.
A pilot will take place across Wakefield and North Kirklees to target 19 optometrist (eye care) practices to enable them to refer direct through an electronic referral process. Although optometrists are also healthcare professionals, they are currently unable to refer people directly into hospital eye services and this creates additional pressure for GPs who are required to send referrals on behalf of the optometrists. This process can result in delays for people in the time taken for their referral to reach hospital eye services. The pilot scheme will allow optometrists to refer people directly into hospital eye services. They will receive technical training and support provided by NHS Digital prior to roll out commencing.
The eRS pilot will run for six months. If successful, it is expected that eRS for community optometrists will be rolled out nationally and across West Yorkshire and Harrogate in phases, to be completed by the end of 2019. The Partnership’s planned care programme will be working closely with NHS England and NHS Digital to make sure that the roll out across West Yorkshire and Harrogate follows the national scheme and addresses any issues coming out of the local pilot scheme.
The deadline for submitting the estate strategy to NHS England is approaching and Catherine Riley, programme lead for estates and strategy is working with other colleagues across the area to develop a draft plan. This will be shared with the leadership group for their views ahead of submission.
There was also an update on GP contracts, primary care networks / communities and funding. The primary care workforce group met this week – this included local area colleagues as well as those from Health Education England. The NHS App provides a simple and secure way for people to access a range of NHS services on their smartphone or tablet. It is being rolled out across the area.
Harnessing the power of communities
In 2018, the Partnership allocated £1m to go toward supporting organisations to help tackle loneliness through our 'Harnessing the Power of Communities Programme' led by Soo Nevison, CEO for Community Action Bradford and District. Community and voluntary partners were allocated additional resources through their partnership work with local councils and the Health and Wellbeing Boards. This includes Leeds Community Foundation who received funding from the programme and NHS Leeds. Both the initial report and the recent update report can be downloaded from their website here. We are gathering information from all organisations funded and will promote the difference these projects have made to people’s lives on our website in the coming weeks. You can find out more here.

