Posted on: 31 March 2023
 Hello, my name is Becky
Hello, my name is Becky
I am the Associate Director for Partnerships and System Development for the Wakefield District Health and Care Partnership (WDHCP). I’ve been doing this job for about eighteen months.
Before staring in this role I had worked at Leeds CCG for many years in various roles. My new role in Wakefield was similar enough to what I had been doing in Leeds to feel like familiar territory – I was only moving next door, right? I was even sitting at the same desk in my spare bedroom for the majority of the time. How different could it really be?
Answer: really different! Yes, the context was broadly the same, and most of the subject matter was identical but somehow it felt completely alien initially. It confirmed something that we all know; that it’s people, relationships and networks that are at the heart of how we work and what we do. We all add something individual to that which creates a unique mix. These are things that you cannot see on a governance chart or in an operational model, but they are the things that drive our culture and purpose.
Thankfully my new colleagues were welcoming and patient and it didn’t take too long for me to feel like part of the family.
It’s been a really enjoyable journey being part of developing the Wakefield District Health and Care Partnership over the past eighteen months and I’ve been struck by the strength of the relationships that exist here.
The relationships that exist in WDHCP have been built slowly and carefully over many years, involving a huge commitment to partnership working by individuals and organisations, often setting organisational interests aside for the wider purpose of making improvements for the local population. There have been similar journeys in all our places.
What binds us together more than anything is our local Health and Wellbeing Strategy. This provides us with the ultimate goal for our residents and the perfect mechanism to facilitate partnership working in our place. Health and Wellbeing Strategies are the umbrella for each of the places in West Yorkshire allowing us to focus on the specific needs of our people and communities.
For me, my move from one place in West Yorkshire to another has highlighted the West Yorkshire Health and Care Partnership’s principle of subsidiarity. This is vitally important to enable places to continue to build these local relationships and work for our populations.
At the same time this can be balanced effectively with the benefits of working at scale across West Yorkshire where it makes sense to do so. All the five places are different but there is great strength in harnessing that diversity. All the evidence tells us that where we come together to do this effectively, we become excellent problem-solvers and innovators.
 A good example of this working in practice is the West Yorkshire Health and Care Partnership Strategy Development Group, which I have been part of for the past year or so, alongside colleagues from each of the places as well as from the ‘central’ ICB teams. The purpose of the group was to co-produce together the West Yorkshire Integrated Care Strategy and Joint Forward Plan but to do this in a way that builds from what’s most important to the five places.
A good example of this working in practice is the West Yorkshire Health and Care Partnership Strategy Development Group, which I have been part of for the past year or so, alongside colleagues from each of the places as well as from the ‘central’ ICB teams. The purpose of the group was to co-produce together the West Yorkshire Integrated Care Strategy and Joint Forward Plan but to do this in a way that builds from what’s most important to the five places.
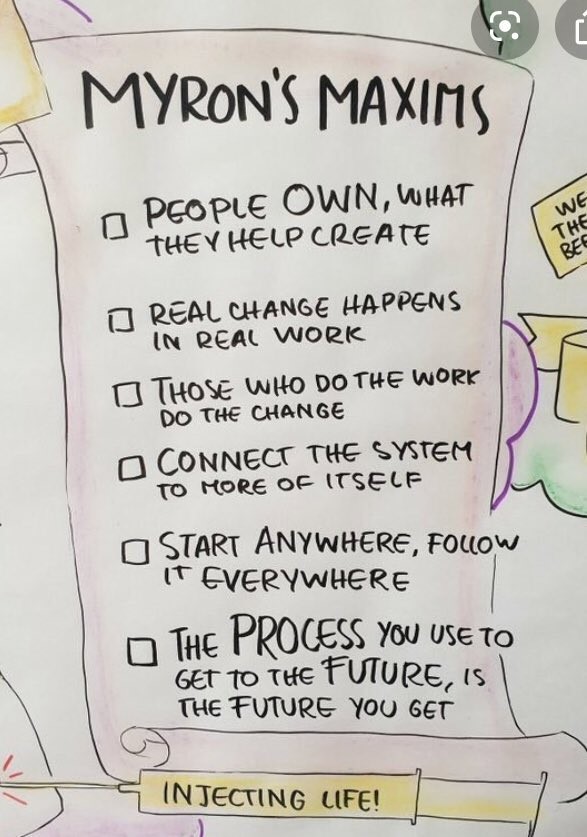
We’ve been lucky enough to be supported by Myron Rogers in every session and this has led to quite a radical approach to the work, which we have all enjoyed as well as being challenged by at times. For example the ‘fish-bowl’ method of ensuring all voices are heard and exploring knotty issues in a respectful way has been really effective.
The group has built into a network and involves many colleagues from across the patch and it’s been so valuable to build up a wider set of relationships and also to take some of the approaches and techniques back into our places.
‘Myron’s Maxims’ have been a constant presence in each of the sessions. They are all pertinent but the one that always particularly resonates with me is ‘the process you use to get to the future is the future you’ll get’. If we continue to put relationships and people at the heart of what we do and continue to value the differences we have, I do feel optimistic.
What else has been happening this week?
Pre-election period
Our integrated care board, as well as other NHS and public sector organisations, is now in a period of pre-election restrictions. In effect until the ballots close on Thursday 4 May 2023, the pre-election period is designed to avoid the actions of public bodies distracting from or having influence on election campaigns.
This means, for example, there should be:
- No new announcements of policy or strategy
- No announcements on large and/or contentious procurement contracts
- No participation by NHS representatives in debates and events that may be politically controversial, whether at national or local level
- Nothing contentious posted on websites or social media accounts. Updates/posts, including blogs, should only convey essential factual information.
The pre-election guidance for NHS bodies is available on the NHS England website. For local authorities, there’s information on the Local Government Association website and guidance for civil servants can be found on the gov.uk website. The guidance also applies to Healthwatch organisations – there’s more information on Healthwatch England’s website.
If you’re unsure about whether any activity you’re undertaking during the pre-election period is subject to this guidance, please contact your organisation or place-based ICB communications team.
West Yorkshire’s NHS eating disorders service retains quality mark from Royal College
 Adults with eating disorders across West Yorkshire are receiving top quality treatment according to national experts.
Adults with eating disorders across West Yorkshire are receiving top quality treatment according to national experts.
The Yorkshire Centre for Eating Disorders (YCED) has retained its accreditation to the Quality Network for Eating Disorders (QED), a national quality mark from the Royal College of Psychiatrists.
The YCED treats the most acutely ill people with eating disorders from across our region. This 14-bed unit based at the Newsam Centre in Seacroft, Leeds, treats around 35 inpatients a year including adults with anorexia and bulimia.
 Michelle Leary-Simmons, Inpatient Clinical Team Manager at the Yorkshire Centre for Eating Disorders, said:
Michelle Leary-Simmons, Inpatient Clinical Team Manager at the Yorkshire Centre for Eating Disorders, said:
“We’re the first nurse-led inpatient eating disorder service in the country with accreditation from the Royal College of Psychiatrists. It’s a privilege to be part of a team that is not only pioneering but always striving to towards excellence to meet the needs of patients with eating disorders. High quality patient care is always at the heart of our practice. Retaining this accreditation shows that we’re continuing to achieve this.
The accreditation process itself was challenging but ultimately rewarding as it’s enabled us to show to others what we do well and how we can adapt to deliver even better. We’re a diverse team consisting of a Nurse Consultant, psychologists, occupational therapists, nurses and dietitians who work well together with patients to provide safe, reliable and effective care. Well done team!”
Autism Acceptance Week
This week is Autism Acceptance Week. Across West Yorkshire, the Partnership aims to achieve a 10% reduction in the gap in life expectancy between people with mental ill-health, learning disabilities and autism/neurodiversity, and the general population. Achieving this ambition will make life better for more than 200,000 people living in West Yorkshire. This video has been made by a group of young people who have helped us with our work and explains what life can be like for neurodivergent people.
Our ambition is to make the best use of our collective expertise, including lived experience, to improve services, influence the wider determinants of health and in particular address social inequalities faced by neurodivergent people or those seeking a diagnosis of autism and/or ADHD.
New pathology laboratory reaches new milestone
Construction of Leeds Teaching Hospitals NHS Trust’s new state-of-the-art pathology laboratory has reached a new milestone, bringing it a step closer to transforming diagnostic services right across West Yorkshire.
BAM has now completed the outer shell of the building, which is based at the Trust’s St James’s University Hospital (SJUH) site, with all the windows now fitted using 338 pieces of glass. A further 1,357 individual rainscreen cladding panels have also been fitted to the façade and it is now on track to be operating with power in the coming weeks. You can watch a time-lapse video of the building progress here.
Currently, most of the Trust’s pathology services are delivered from outdated facilities in the Old Medical School at the Leeds General Infirmary (LGI) as well as from St James’s Hospital.
The new building will bring many of these services together into one purpose-built facility and once vacated, the Old Medical School will be repurposed as part of a plan to use surplus estate at the LGI to develop an innovation village which is expected to deliver up to 4,000 new jobs and almost £13bn in net present value.
Bringing these pathology services together into the new building will support the delivery of faster, more accurate routine and specialist testing and will help to drive improvements in diagnosis for patients across the region.
The new laboratory will be part of the West Yorkshire and Harrogate Pathology Network, formed through the collaboration with the West Yorkshire Association of Acute Trusts (WYAAT).
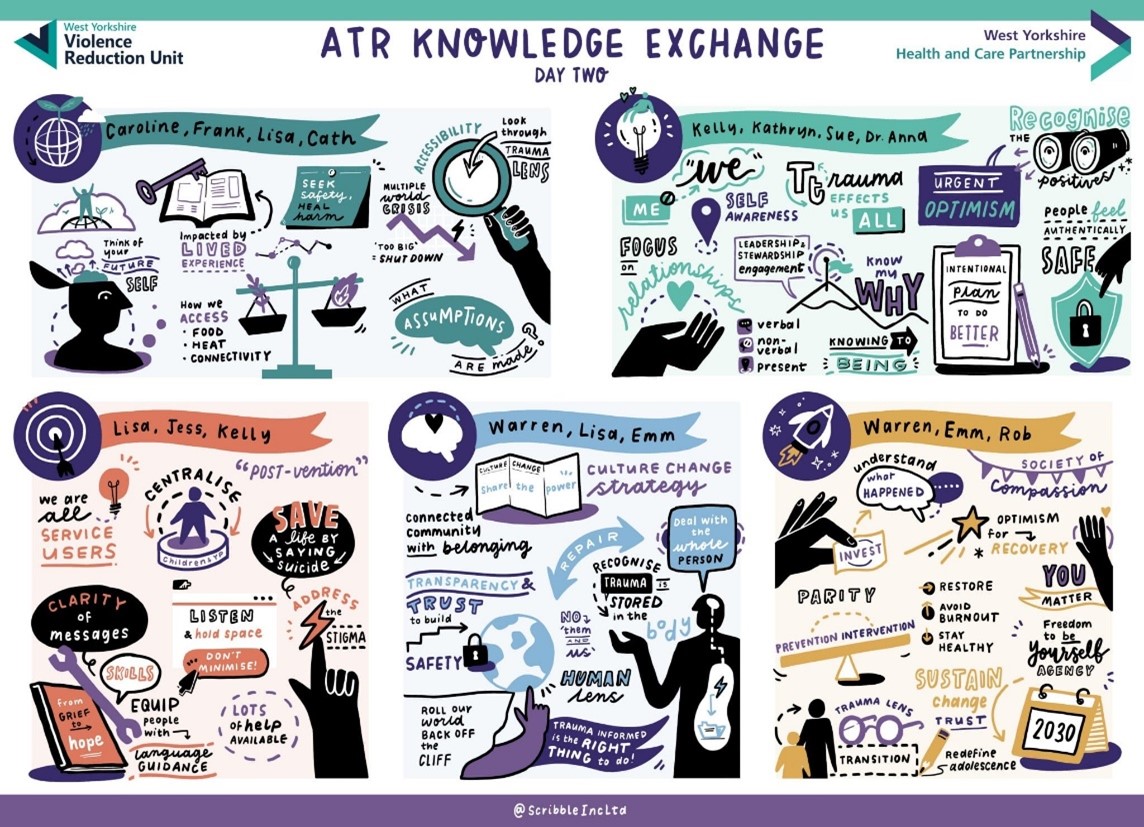
Catch up with our third annual Adversity, Trauma and Resilience Knowledge Exchange
The recordings from our third annual Adversity, Trauma and Resilience Knowledge Exchange held in partnership with the West Yorkshire Violence Reduction Unit from Tuesday 21 to Thursday 23 March are now available.
 See the event website for the full line up and more information about the speakers. To view all the recordings from the event, click on the agenda tab and select which recording you want to see. You can also sign up to our digital hub, which brings together resources to support trauma informed health and care.
See the event website for the full line up and more information about the speakers. To view all the recordings from the event, click on the agenda tab and select which recording you want to see. You can also sign up to our digital hub, which brings together resources to support trauma informed health and care.
How to embed trauma informed practice across the public sector
Inside Government hosted an event to explore work on embedding trauma and resilience programmes across the public sector this week. Emm Irving, Senior Programme Manager for Improving Population Health, chaired the virtual event and also led a session around creating a regional approach to delivering trauma-informed services.
Improving Population Health Programme (IPHP) Board
The programme purpose and priorities was the first topic for discussion at this week’s Improving Population Health Programme Board on Wednesday. The purpose of the programme to work across the NHS and with partners to improve health outcomes, tackle inequalities, support social and economic development and enhance productivity and value for money remains unchanged.
Members agreed the five main programme priority areas which are:
- Reducing health inequalities including CORE20Plus and targeted prevention
- Climate change
- Adversity, trauma and resilience
- Core determinants of health including housing, economy and transport
- Suicide prevention
 Members gave a warm welcome to Jen Connolly who joined her first IPHP Board since joining the Partnership last month to take up the Associate Director of Population Health - Core Determinants role. This is a joint role between the Integrated Care Board (ICB) and the West Yorkshire Combined Authority (WYCA) to support our ambitions to improve population health and reduce health inequalities. Jen is currently working closely with interim Associate Director, Fredi Garbe and will work with Associate Director, Sarah Smith when she returns from maternity leave in May.
Members gave a warm welcome to Jen Connolly who joined her first IPHP Board since joining the Partnership last month to take up the Associate Director of Population Health - Core Determinants role. This is a joint role between the Integrated Care Board (ICB) and the West Yorkshire Combined Authority (WYCA) to support our ambitions to improve population health and reduce health inequalities. Jen is currently working closely with interim Associate Director, Fredi Garbe and will work with Associate Director, Sarah Smith when she returns from maternity leave in May.
Next, members considered a report describing the actions being taken by the West Yorkshire Housing Partnership (WYHP) to make sure that people in social housing in our region do not experience ill-health as a result of condensation, damp and mould. The WYHP is made up of 14 members – 12 housing associations and two stock holding local authorities.
WYHP has shared best practice and identified areas for improvement including developing robust procedures for capturing and responding to cases of damp and mould. Recommendations included making sure that we explore home environments and conditions with patients and agree pathways for further support on housing.
The Cost of Living Steering Group set out the collective actions agreed by the Partnership and WYCA in response to the impact of the cost of living. This includes reducing costs to households, providing support to employees in financial hardship, supporting voluntary and community sector organisations and ensuring mental health and suicide prevention services are providing appropriate support.
This month’s board was chaired by Robin Tuddenham, Place Lead for Calderdale for NHS West Yorkshire Integrated Care Board, CEO for Calderdale Council and Joint Senior Responsible Owner (SRO) of the Partnership’s Improving Population Health Programme.
Urgent and emergency care programme Board
The urgent and emergency care programme board (UEC) met on Tuesday 14 March and was chaired by Clare Smith, Chief Operating Officer at Leeds Teaching Hospital NHS Trust, and the programme’s new Senior Responsible Officer.
A refresh of the UEC programme is currently underway as several projects had reached a natural conclusion. This has provided an opportunity to realign the priorities of the programme to reflect those of the West Yorkshire Integrated Care Board (WY ICB) and the recently published national guidance on UEC recovery. Jon Parnaby, Transformation Programme Manager for UEC at Kirklees Place, was thanked for taking a lead on shaping the refreshed West Yorkshire UEC priorities and for supporting the UEC programme team.
The Board received updates on winter learning, the programme’s contribution to the West Yorkshire Joint Forward Plan, the Y&H Integrated Commissioning Forum and patient discharge.
The Board signed off the programme’s priorities, which have been updated to align with the UEC Recovery Plan. The four key objectives for the next two years include:
- Further development of the West Yorkshire Clinical Assessment Service (WY CAS)
- West Yorkshire urgent care service review
- Same day emergency care (SDEC) developments at scale
- Support to Yorkshire Ambulance Service transformation
Plans on pages will be developed for each of the new priorities which will include metrics, outputs, and associated outcomes.

