Posted on: 24 September 2021

It’s a slightly different approach for this week’s leadership message, as we mark the end of an era for the West Yorkshire and Harrogate Cancer Alliance, and the beginning of an exciting new chapter alongside the proposed changes to the Integrated Care System.
Professor Sean Duffy and Carol Ferguson, who have spearheaded the development of our Cancer Alliance from day one as Clinical Lead and Programme Director respectively, will be retiring at the end of the month, leaving a huge legacy in cancer services both regionally and nationally. Their contributions not only to cancer but also to the wider NHS have helped to position West Yorkshire and Harrogate as a national exemplar in terms of partnership and collaboration, as well as supporting innovation and transformation in service delivery and patient experience.
As the Alliance moves forward into a new chapter, Jason Pawluk joins the team as its new Programme Director and brings to the role a wealth of experience in strategic and operational cancer service management, improvement and wider transformation across London and the North West of England. Jason was latterly Delivery Director for the NHS Transformation Unit, working across the Manchester area.
Recruitment to the post of Clinical Lead is continuing and interim arrangements following Sean’s retirement remain under discussion.
Ian Holmes, Director for the Health and Care Partnership, said:
“Sean and Carol have made a huge contribution to improving cancer services in our region over the last two decades. They have also been mainstays of our integrated care system since day one. They will both be missed hugely but leave a strong legacy for the future of the alliance.”
Sean and Carol were instrumental in establishing the WYH Cancer Alliance five years ago, when 19 such Alliances were established by NHS England to implement the recommendations of the independent national cancer taskforce in its report of May 2016. Their primary role was to steer the Cancer Alliance in its work to determine how national funding should be invested in a transformation programme to improve survival, early diagnosis, patient experience and long-term quality of life across a whole population; to reduce variability in care and treatment; to pilot innovative approaches and to share best practice. But this wasn’t the first iteration of this formidable working partnership. Sean and Carol had already worked closely together in a previous life, both at national level and also within the Yorkshire Cancer Network – in many ways the forerunner of the Cancer Alliance.
Rob Webster, CEO Lead for our Partnership recalls those early days on the patch.
Said Rob:
“I first worked with Sean and Carol when I chaired the Yorkshire Cancer Network from 2007-2011. Their passion for excellence, support for clinical leadership and firm commitment to coproduction with people were obvious from day one. Their support for the Network meant that cancer services and treatments improved every year. They subsequently took their skills to national roles before we welcomed them back to run our Cancer Alliance in West Yorkshire and Harrogate. Many things had changed in health and care while they had been away, yet they were a welcome constant, unchanged in their visible leadership and ambition for things to keep getting better.”
Sean and Carol’s long-standing clinician/manager partnership began in 2005 when Sean became Clinical Director of the Yorkshire Cancer Network and was cemented further when Sean was appointed as National Clinical Director for Cancer in 2013 and Carol was released on secondment to provide senior management support. They have each brought differing but strong and complementary career backgrounds and skills to their working partnership over the years.
A Professor of Healthcare Innovation in Cancer, Sean has many years’ experience as a clinician, manager and leader, using his academic interests in health services research to underpin his wide variety of roles. His strong platform of research work also encompasses medical education, along with endometrial pathology. Sean has been awarded a number of lectureships and travelling fellowships and in 2002, he became a Fellow of the Royal College of Gynaecologists, in recognition of his contribution to the advancement of the science and practice of obstetrics and gynaecology.
He has been extensively involved in the design and development of undergraduate teaching in Yorkshire, more specifically as a former Director of Learning and Teaching for the School of Medicine at the University of Leeds. Alongside his work as Cancer Alliance Clinical Lead for the past five years, Sean has also been the Strategic Clinical Lead for the Leeds Cancer Centre and Senior Clinical Lead for the West Yorkshire and Harrogate System Leadership Executive. Sean is also retiring from his clinical practice in gynaecology services at Leeds Teaching Hospitals NHS Trust, where he was also a Clinical Director between 2002 and 2007.
Until earlier this year, Sean was External Senior Clinical Advisor to the External Quality Assurance Programme for Cancer with Health Improvement Scotland. He is also a former Chair of both the Cancer and Blood Programme of Care and Specialised Cancer Clinical Reference Group with NHS England.
As in his role as National Director, Sean was central to the development of the 2016 cancer strategy, Achieving World Class Outcomes, covering both specialised and non-specialised services. His strong clinical leadership, extensive networks and political astuteness stood him in great stead. His skills in translating complex issues into plain language, his natural affinity for public speaking and his approachable manner made him an ideal spokesperson for NHS England to the community at large. This has continued into his role with the Cancer Alliance.
Possibly the greatest element of the legacy left by Sean and Carol is the impact of their influence on policy making at national level. Partnership and collaboration has been at the heart of all their work together. During Sean’s time as National Clinical Director, they formed a collaboration with Cancer Research UK and Macmillan, which became the ACE programme, out of which grew the significant national policy priorities around the expansion of Rapid Diagnostic Centres and Targeted Lung Health Checks, bringing huge benefits to patients around the country.
Carol’s authoritative yet understated management style has played a huge part in developing the Alliance’s extensive networks across the whole of the partnership. “I’ve always been particularly interested in a management style that encourages people to deliver because they want to, not because they have to, so working in networks and systems outside of conventional organisational boundaries and hierarchies is of particular interest,” she said.
Carol began her career as a professional health economist in the Department of Health and then the University of York. She moved into the NHS in 1989 and worked in a variety of roles covering data analysis, general management, planning, service redesign and commissioning in regional, local health authority and primary care organisations. Having grown up in a family significantly affected by cancer, her professional involvement came following the publication of the Calman-Hine Report in 1995, when she took the planning lead for its implementation in North Yorkshire.
In April 2001, she joined the Yorkshire Cancer Network as led for service improvement and redesign, and subsequently became the network’s lead manager. Having been told by her then Chief Executive that it couldn’t be a long-term career move, Carol loved the work so much that she stayed until networks were dissolved in 2013. In December of that year, she was released on secondment to support Sean in his role as National Clinical Director, working as part of a small cancer programme team at NHS England. Her three years working at national level taught her a huge amount about politics at that level in both the statutory and third sector.
Sean and Carol are both looking forward to their retirement – but with very different ideas about how they will spend it.
Sean is planning to continue his passion for gardening, and ultimately to return with his wife to their Irish homeland with a move to West Cork and regular visits by their two grown-up sons.
Together with her husband Brian, Carol will be spending more time at their holiday lodge by the sea in North Yorkshire, joined whenever possible by their son and daughter and their respective partners. Already known to many of her colleagues as a great animal lover, Carol will be enjoying lots of long beach and country walks with her beloved rough collies and hacking around the villages on her horse, Casper the Cob.
 In taking over the reins for West Yorkshire and Harrogate, Jason said he was excited to be joining the Cancer Alliance at such pivotal point in its development as part of the wider Health and Care Partnership.
In taking over the reins for West Yorkshire and Harrogate, Jason said he was excited to be joining the Cancer Alliance at such pivotal point in its development as part of the wider Health and Care Partnership.
“It’s clear that so much has been achieved so far, through the direction of the Cancer Alliance Board, the leadership of Sean and Carol, and the commitment, creativity and innovation of place-based teams. It’s great to be arriving at such a crucial and interesting time for the wider Integrated Care System, with the opportunities it presents for collaboration across programme areas and improving overall population health and wellbeing.
I’m really looking forward to getting to know our colleagues across the patch, understanding what matters most to people directly affected by cancer in West Yorkshire and Harrogate, and to focus on delivering the continuing transformation in cancer care and outcomes locally.”
Having graduated from the University of Oxford with a Degree in Modern History, he went on to complete a Masters in Healthcare Management and Leadership at the Universities of Birmingham and Manchester, before joining the NHS Management Training Scheme (MTS). Amongst his early experiences was time spent in New Zealand on an MTS study programme, where he gained experience of working in health promotion for older people, and he retains strong interests in healthcare policy and leadership development.
Jason worked in cancer services for nine years in operational, change and strategy roles before moving to his previous role in the NHS Transformation Unit. His work included spells with the South West London Cancer Network, Guy’s and St. Thomas’ NHS Foundation Trust, St. George’s University Hospitals NHS Foundation Trust and The Clatterbridge Cancer Centre NHS Foundation Trust. He’s been particularly proud to work on capital redevelopment programmes resulting in new state-of-the-art Cancer Centres at Guy’s Hospital and the new Clatterbridge site in Liverpool in particular.
During his time at Clatterbridge, and as Strategic Cancer Networks were coming to an end, Jason helped to set up the Cheshire and Merseyside Cancer Alliance, working with local stakeholders to deliver the policy direction around the independent cancer taskforce report, mirroring the approach which was taken here in West Yorkshire and Harrogate.
In 2018, Jason joined the NHS Transformation Unit as Delivery Director, an internal NHS consultancy role, where he led several high-profile projects, including a planned reconfiguration of hospital services in Central Lancashire.
Jason was born in the North West, and currently lives in Warrington. In his spare time, he enjoys cricket and can be found on a summer weekend afternoon in one of the many parks in Cheshire, standing in the middle and donning a white coat whilst umpiring a game. Jason was keen to point out, however, that whilst he is delighted to be taking up a role on the other side of the Pennines, his main hobby beyond the short British summer - loyalty to Rochdale Football Club - will be staying firmly as it is!
In welcoming Jason and thanking Sean and Carol, Rob Webster said:
“I believe I speak for colleagues across our partnership, our partners and the patients who work alongside us in transforming services and improving care, as I thank Sean and Carol for everything they have done for people in West Yorkshire and Harrogate. I will really miss them.”
“Jason is a very welcome addition to the team who, together with our new Clinical Lead once appointed, is strongly placed to use his own experience and leadership style to take the Cancer Alliance forward as part of a strengthened and redesigned ICS.”
What else has been happening this week?
Let's DiaBEAT this
 Around 45 practice nurses and health care colleagues attended our online Let’s DiaBEAT this event on 22 September to find out the crucial role they can play in preventing type 2 diabetes. We held the event as part of a range of activities to support our Let’s DiaBEAT this campaign and help boost referrals to the NHS Diabetes Prevention Programme. We’ll be doing more formal evaluation but there’s been some great initial feedback including “Brilliant lived experience of NDPP – John’s hard work is an inspiration,” “Very informative sessions. Brilliant work,” “Thank you fab programme," “Had never considered the impact on diabetes prevention and climate change before today - and how we can all do our bit” and “I refer to NDPP regularly but I will now encourage patients to do the Know Your Risk tool too.”
Around 45 practice nurses and health care colleagues attended our online Let’s DiaBEAT this event on 22 September to find out the crucial role they can play in preventing type 2 diabetes. We held the event as part of a range of activities to support our Let’s DiaBEAT this campaign and help boost referrals to the NHS Diabetes Prevention Programme. We’ll be doing more formal evaluation but there’s been some great initial feedback including “Brilliant lived experience of NDPP – John’s hard work is an inspiration,” “Very informative sessions. Brilliant work,” “Thank you fab programme," “Had never considered the impact on diabetes prevention and climate change before today - and how we can all do our bit” and “I refer to NDPP regularly but I will now encourage patients to do the Know Your Risk tool too.”
Attendees heard from a fabulous range of speakers including:
- Adele Graham, Diabetes Programme Manager, West Yorkshire and Harrogate Health and Care Partnership
- Rachel Martin, Improving Care Manager, Diabetes UK– North East and North Cumbria
- Jon Scott Operations Manager, Reed Wellbeing
- Dr Waqas Tahir, Clinical Diabetes Lead, West Yorkshire and Harrogate Health and Care Partnership and Bradford District and Craven System Programme
- Dr James Thomas, GP Partner, Clinical Chair of Bradford District and Craven Clinical Commissioning Group, Chair Clinical Forum West Yorkshire and Harrogate
- Frank Swinton, Climate Change Lead
- John Ebo, NDPP patient
Seeking patients’ views on elective recovery
The NHS Confederation is publishing a report on the future of the health and care system, based on a survey of 100 leaders across all parts of the system. A big focus of this report will be around recovering the backlog of elective care in ways that don’t exacerbate health inequalities. This short case study on the Partnership's Planned Care Citizens' Panel will feature in this report.
Case study
 Our Planned Care Citizens’ Panel was introduced in partnership with Healthwatch to support communications around elective recovery in West Yorkshire and Harrogate. The panel of volunteers from across the area, all patients on the waiting list for elective care, was in place from June to September 2021.
Our Planned Care Citizens’ Panel was introduced in partnership with Healthwatch to support communications around elective recovery in West Yorkshire and Harrogate. The panel of volunteers from across the area, all patients on the waiting list for elective care, was in place from June to September 2021.
Panel members met online every two weeks when clinicians and other colleagues from across the
Partnership shared details with them about how we are working together as a system to reduce the backlog of elective cases resulting from the pandemic.
All panel members were extremely keen to support elective recovery work and help improve the situation for others in the same position. They shared their own experiences of waiting, asked relevant questions, and provided valuable insight around several areas of healthcare, not just elective recovery.
Themes included patient and public communications, personalised care, shared decision-making, clinical validation, prioritisation of patients, proposals for creating additional elective capacity, and the current pressures on accident and emergency services.
One of the most important themes for panel member was around helping patients to stay well during their wait for care so support services, such as patient information and guidance, social prescribing options and activities provided by the VCSE sector were also covered.
All this comprehensive feedback is now being used by the appropriate programmes and teams within the Partnership for ongoing consideration as work progresses.
We are now looking at how we can keep panel members involved with these important work areas, to make sure that the voice of the patient is heard, and to retain the personal experiences and knowledge that only people with a lived experience can bring.
Improving Population Health Programme Board
 The Improving Population Health Programme Board met last Friday. The board reflected on the latest activities across climate change, diabetes, housing for health, health inequalities, prevention and reducing violent crime. Representatives from Nova, which provides a range of services for the voluntary, community and social enterprise (VCSE) sector in the Wakefield district, explained how they’ve been making a difference through funding for their Hub Pantry Project. The board heard about how we are working together to help empower refugees and asylum seekers to access welcoming and safe healthcare, as part of our ambition to become the first ‘Integrated Care System of Sanctuary.’
The Improving Population Health Programme Board met last Friday. The board reflected on the latest activities across climate change, diabetes, housing for health, health inequalities, prevention and reducing violent crime. Representatives from Nova, which provides a range of services for the voluntary, community and social enterprise (VCSE) sector in the Wakefield district, explained how they’ve been making a difference through funding for their Hub Pantry Project. The board heard about how we are working together to help empower refugees and asylum seekers to access welcoming and safe healthcare, as part of our ambition to become the first ‘Integrated Care System of Sanctuary.’
There were also updates on our work to tackle violence against women and girls, long term prevention planning and health inequalities funding.
The board is chaired by Dr James Thomas, Chair of Bradford District and Craven Clinical Commissioning Group and Robin Tuddenham, CEO for Calderdale Council and Chief Officer for Calderdale Commissioning Group.
Mental Health, Learning Disabilities and Autism Programme Board
The Mental Health, Learning Disabilities and Autism Programme Board met recently to discuss the Workforce Strategy. The Strategy has been developed further with working group input, including ways to attract recruits from local communities and using clearer language for job descriptions to help open-up interest and diversity of applicants. Two events are coming up as part of the Strategy – the Partnership’s first virtual recruitment Fair takes place on 30 September with a focus on mental health professions and roles. The Fair is open to all and free to attend. You can find out more about the recruitment fair here. The ‘Future Workforce Solutions for Mental Health and Learning Disabilities services’ event takes place on 15 October, to give colleagues the opportunity to find out more about some of the new emerging professional roles in mental health and learning disability services, focusing on how these roles offer valuable future workforce solutions to enhance our workforce models and improve our services. To find out more and book a place click here.
The Board received project updates about perinatal mental health, suicide prevention and autism. Specialised Services continue to progress new models of care for adult eating disorders, child adolescent mental health services (CAMHs) and forensic services via lead provider collaborative arrangements. Adult secure and CAMHs will go live next week (1 October). More information about these new arrangements will be communicated shortly.
Health Equity Fellowship
 As part of our Health Inequalities Academy work, we are developing a Health Equity Fellowship Programme for West Yorkshire and Harrogate. Initially, there will be 30 places on offer and applications from employees across the partnership will be welcome. We’ll expect fellows to dedicate one day a week of their time to attend health equity training and work on a health equity project.
As part of our Health Inequalities Academy work, we are developing a Health Equity Fellowship Programme for West Yorkshire and Harrogate. Initially, there will be 30 places on offer and applications from employees across the partnership will be welcome. We’ll expect fellows to dedicate one day a week of their time to attend health equity training and work on a health equity project.
Successful applicants can deliver projects in their usual place of work or it could be something that contributes to wider integrated care partnership or integrated care system approaches. Watch out for more details, including how to apply, soon.
Fuel poverty
 Every winter, thousands of people are faced with the hard decision of whether to buy food or use that money to heat their homes. According to 2018 government statistics, there are over 100,000 households in fuel poverty across West Yorkshire and Harrogate alone.
Every winter, thousands of people are faced with the hard decision of whether to buy food or use that money to heat their homes. According to 2018 government statistics, there are over 100,000 households in fuel poverty across West Yorkshire and Harrogate alone.
We have produced a fuel poverty infographic, aimed at people working in health and care services, that details the groups of people most likely to experience negative health impacts of fuel poverty and the signs to look out for. In addition, there is a fuel poverty leaflet for people who are living in fuel poverty and struggling to afford their energy bills.
The leaflet contains links to support services and information about the different benefits and grants available to help people get out of fuel poverty and experience better health.
Check-in Suicide Prevention Campaign
 Over 650 people have taken part in the zero-suicide alliance training since the launch of the Check-In Campaign in February.
Over 650 people have taken part in the zero-suicide alliance training since the launch of the Check-In Campaign in February.
You can read the latest Check-in evaluation report here for this award-winning campaign.
Organ Donation Week
 To mark our support, we would encourage everyone to tell their family their organ donation decision and record it on the Organ Donor Register.
To mark our support, we would encourage everyone to tell their family their organ donation decision and record it on the Organ Donor Register.
Together, we can raise awareness for organ donation in our communities.
Looking out for each other
 On 13 September our #SpreadTheKindness campaign officially launched and the number of supporters signing up continues to grow. On Tuesday 21 September we shared the first video titled ‘spread the kindness’ produced by the campaign ambassadors. The videos will be shot in TikTok style and will be shared as reels on TikTok and Instagram to capture the interest of young people.
On 13 September our #SpreadTheKindness campaign officially launched and the number of supporters signing up continues to grow. On Tuesday 21 September we shared the first video titled ‘spread the kindness’ produced by the campaign ambassadors. The videos will be shot in TikTok style and will be shared as reels on TikTok and Instagram to capture the interest of young people.
We hope the campaign will reach as many young people as possible. To help us do this the campaign ambassadors will be working alongside universities, carers organisations, LGBTQ+ support groups and other community groups associated with young people across West Yorkshire and Harrogate. Please continue to encourage organisations/support services working alongside young people sign up at: http://ourneighbours.org.uk/eachother/ .They will receive a follow up telephone call about how they could potentially use the resource pack once they have completed the online form. For more information please contact: Vicky.
Urgent and Emergency Care Programme Board
The urgent and emergency care programme board (UEC) met on Tuesday 21 September.
The West Yorkshire UEC Dashboard is in the final stages of development. Weekly meetings are taking place between North East Commissioning Support Unit (NECS) colleagues and the UEC data analyst to support the handover of the dashboard. A 111 Online clinical validation pilot has been completed in Leeds and this is where people who have used NHS 111 online and have been recommended to go to an emergency department are asked if they would like a call back from a clinician to see if there may be other alternatives following the conversation which will take place. It is hoped that once this pilot has been completed and evaluated, 111 online clinical validations will be rolled out to the rest of West Yorkshire.
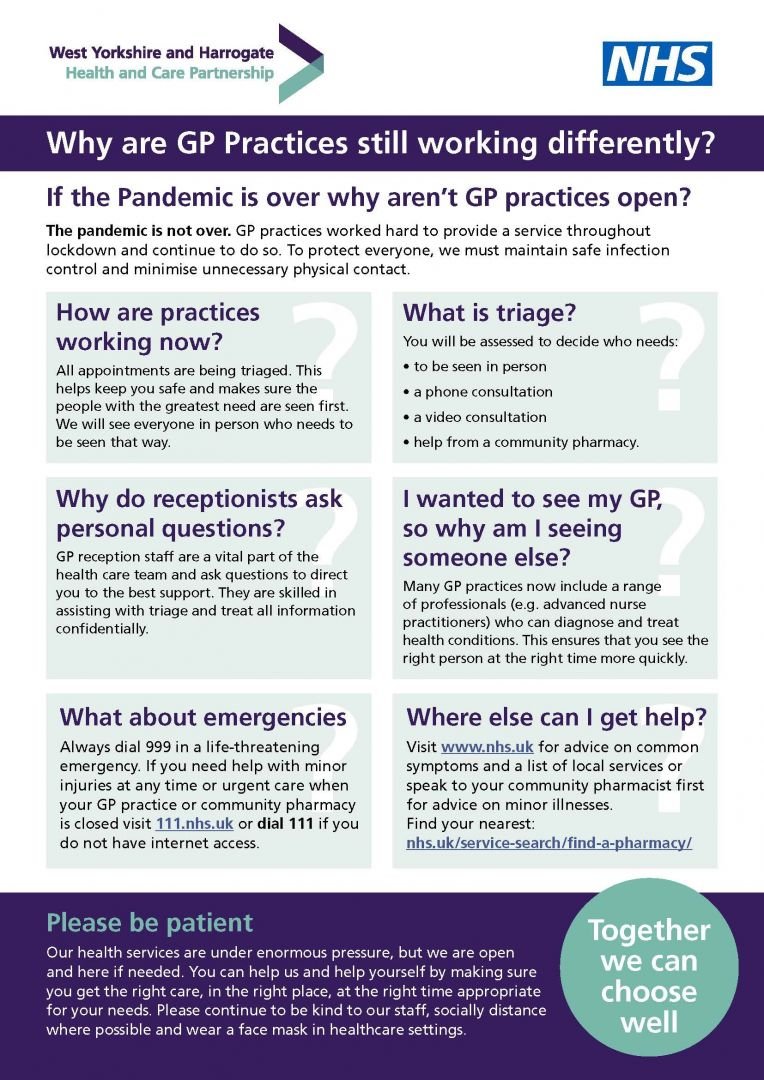
The board welcomed the distribution of an infographic to help explain more about ‘Why are GP practices still working differently?’ In response to ongoing patient need and public perceptions about the ways in which primary care continues to operate.
Andrew Nutter, Deputy Chief Executive and Chief Operating Officer of Local Care Direct (LCD) shared an update with the board. The presentation focused on the development of a local Clinical Assessment Service (CAS) offering, delivered by Local Care Direct, to support achievement of the aims of the 111 First initiative. He also outlined some next steps and opportunities to develop additional 111 First/Local CAS pathways and options for managing face to face needs in daytime.
In light of the pandemic recovery as well as the circumstances this winter will bring, the board heard that the Partnership, working largely through our local places, will need to demonstrate a robust process to winter plans this year. This includes implementing a 10 point action plan to mitigate urgent and emergency care pressures. We will be working to ensure winter plans are integrated at a system level and will be developing a West Yorkshire Winter Plan which will also include work of other programmes across our area.
West Yorkshire Patient Transport Services (PTS) and becoming a national pathfinder region
Sibghat Ullah, Principal Contracts Manager Regional Contracts, NHS Kirklees Clinical Commissioning Group gave a presentation at the urgent and emergency care programme board about West Yorkshire Patient Transport Services (PTS). It's positive news that West Yorkshire has been confirmed as a national pathfinder area as part of the National NHS Non-Emergency Patient Transport Services (NEPTS) review. This followed NHS England and NHS Improvement inviting proposals for testing the implementation of the areas outcome from the review. In preparation to bid to be a pathfinder area, a joint collaborative proposal was developed between West Yorkshire Commissioners and Yorkshire Ambulance Service (YAS) covering key requirements of the programme. The NEPTS Review implementation programme has four components: eligibility criteria, signposting of patients, strengthening community transport, new contracting and procurement principles.
Meanwhile, across West Yorkshire a PTS review is also in progress which has four phases including scoping, system engagement, developing models of collaboration and recommendations and runs from July 2021 to March 2022. The next steps include information collection and a workshop with stakeholders. Regular updates will continue to be shared as this work progresses. For further information please contact sibghatullah
Falls prevention
Falls Prevention week will be held from Monday 27 September to Friday 1 October (coinciding with the International Day of Older People on 1 October). Modelling predicts that 110,000 more older people will have at least one fall a year because of reduced physical activity during the pandemic. Falls and fractures are often preventable and there are several initiatives to reduce this risk. For more information see the Public Health England report and the following resources:
Working together to reduce maternal smoking rates in Wakefield
 Smoking is the most significant cause of health inequalities. For some, the risks start before they are born, with a high number of pregnant women recorded as smokers at time of delivery (SATOD). Wakefield Integrated Care Partnership (ICP) has made significant progress in addressing this, with a drop in maternal smoking rates of almost 10% over 10 years. In 2020/21, 14.6% of pregnant mothers in Wakefield District were smokers, compared to 23.9% in 2010/11. Whilst this remains higher than the national rate of 9.5%, the fall in figures far exceeds the national fall over the same period, of 3.2%.
Smoking is the most significant cause of health inequalities. For some, the risks start before they are born, with a high number of pregnant women recorded as smokers at time of delivery (SATOD). Wakefield Integrated Care Partnership (ICP) has made significant progress in addressing this, with a drop in maternal smoking rates of almost 10% over 10 years. In 2020/21, 14.6% of pregnant mothers in Wakefield District were smokers, compared to 23.9% in 2010/11. Whilst this remains higher than the national rate of 9.5%, the fall in figures far exceeds the national fall over the same period, of 3.2%.
Stopping smoking in pregnancy is the most significant change that can improve the health of a mother and baby. Smoking is the single biggest risk factor for still-birth, and it increases the risk of serious complications during pregnancy and labour, including miscarriage, premature birth and low birth weight. It is linked to sudden unexpected death in infancy and is also associated with respiratory problems such as pneumonia and asthma in babies and infants (which can be fatal). Stopping smoking is the most effective thing we can do to reduce these risks.
Wakefield’s excellent progress is addressing maternal smoking has been achieved through partnership working, with a range of approaches are used across the District. This includes a dedicated specialist midwife, which has been key in providing insights and enhancing links between different organisations and roles.
A Personal Finance Incentive Scheme means pregnant women who set a quit date with NHS Yorkshire Smokefree Wakefield are provided with a Carbon Monoxide (CO) single patient monitor, so they can perform regular CO readings. If they are successful in remaining smoke free, they are issued with shopping vouchers at monthly intervals, until two months after the birth.