Posted on: 11 July 2019
This week’s leadership message comes from Cindy Fedell, Chief Digital and Information Officer for Bradford Teaching Hospitals NHS Foundation Trust. Cindy is also our Senior Responsible Officer for the West Yorkshire and Harrogate Health and Care Partnership Digital Programme
 Hello, my name is Cindy
Hello, my name is Cindy
I have the privilege of being the Senior Responsible Officer for the West Yorkshire and Harrogate Digital Programme. This is a newly created role for the Partnership which recognises, in this day and age, that all things digital play an important part in our lives and hence, in our health and care.
You may think we are miles away from the world of Star Trek and advanced technology. But when you look back at Star Trek you will be amazed at how much we already have in place today. The technology opportunity is real life, here and now, and we are seeing significant uptake – and not just by those of us who have a soft spot for sci-fi or technology.
In West Yorkshire and Harrogate we are setting ourselves a progressive digital ambition or in other words ‘putting technology and data in the hands of our capable people – citizens, patient, carers and staff, to enable us to use its power’. Just like you use technology to buy your train tickets, watch your shows and do your online banking, we want to make the most of the benefits it brings to people’s lives.
The Partnership’s digital ambition is being set through a series of engagement workshops. The first one was held in May and included our Chief Clinical Information Officers (CCIOs) and our Chief Digital and Information Officers (CDIOs) from each of our organisations. These are doctors, nurses, and allied health professionals as well as digital people (like me) that jointly set the direction for all things digital. The workshop was well attended with about 50 leaders coming together to showcase projects and discuss what can be shared and spread, and what more we can do together.
This is of course only part of an important picture – we also need to understand what people accessing health and care think about technology. This is why we welcomed the Healthwatch engagement findings and the recent report on digitisation and personalisation. You can read them here. We are taking these views seriously and are looking at what else we need to do to make these views real for people.
There are many CCIOs and CDIOs specialising in digital work across West Yorkshire and Harrogate. For the Partnership there is me and two lead CCIOs, Dr Justin Tuggey and Dr Alistair Walling. Justin is the CCIO at Airedale Hospital NHS Foundation Trust as well as a Consultant in Respiratory Medicine and their Caldicott Guardian. Alistair is the CCIO at Leeds City Council/Clinical Commissioning Group and is also a Leeds GP. We have a great project team supporting our work led by Dawn Greaves.
So, what are we doing? We are:
- Making access to care easier: We are doing this in various ways, for example through video links using mobile phones and screens in doctors’ surgeries. Another example can be found at Leeds Teaching Hospitals @DitLeeds where the Dermatology Clinics are able to review digital photos. This saves people’s time and travel costs by not having to come into the hospital. They are aiming to reduce face to face follow-up ambulatory visits substantially across their Trust. In Kirklees people can access Council activities through their Alexa. This makes some services easier to access than traditional phone, post and/ or face-to-face appointments. Kirklees Council’s My Kirklees Account has already over 100,000 people registered.
- Giving people the information they need: Firstly, by linking up clinical records from different clinicians when appropriate we are able to provide clinicians with all the information they need about patients to ensure seamless care. Although we currently have several ways of doing this electronically and using paper, we can improve this so that more information is available and faster – benefiting both staff and patients.
There is some great partnership work taking place across the area. For example, electronic shared records, such as in Bradford District and Craven where there are shared patient records between Airedale Hospital Foundation Trust @IHRTeam and Bradford Teaching Hospitals Foundation Trust @BradfordDigital and our GPs and also between Bradford and Calderdale and Huddersfield Trusts @thisnhs and GPs.
Using the Leeds Care Record as a base we are building the Yorkshire and Humber Care Record. The first wave saw Leeds’s records hooked up with records in Humber and South Yorkshire and the second wave will see Bradford connected. Secondly, not just for clinicians, but for all of us including carers, we are providing people with the ability to access their own health care records. This gives people the opportunity to participate in defining their care needs. Across West Yorkshire and Harrogate there are already over 800,000 people accessing their GP record online.
On the topic of better and faster information for clinicians, the Yorkshire Ambulance Service has implemented software in the ambulances whereby their teams can capture information from assessments anywhere they are. This means that information can be shared with hospital doctors and nurses en route to hospital, for example when someone has had a stroke.
Our Partnership is also home to the Yorkshire Imaging Collaborative, led clinically by Dan Fascia from Harrogate NHS Foundation Trust, which is providing direct access for clinicians to every image from anywhere. We are also preparing for the next stage which will see radiologists reporting on those images from anywhere.
- Helping all our organisations become digitally mature: To ensure our workforce and people accessing care have modern tools, supported by good infrastructure, we will drive the implementation of digital tools throughout the Partnership. For example, Mid Yorkshire Hospitals Trust #MyDigitalFuture is implementing electronic prescribing and medicines administration software, which prompts clinicians to potential interactions between drugs and allergies that could cause the person harm.
- Making sure technology is safe, resilient and sustainable: This is all about working together to ensure that whatever we create and implement is not faulty, does not fall over just when we need it, and it will last. An example of this is the Pathology Laboratory Information System (LIMS) which we are looking to put in once for all of us. This will allow us, through economies of scale, to purchase a well-respected tool that is most importantly reliable.
 Using the taxpayer pound efficiently between us: We will ensure that technology can be shared between us rather than buying it more than once. We are looking to see what we can leverage from each other or simply what can we learn and apply without having to relearn. The Scan4Safety project led by Stuart McMillan at Leeds Teaching Hospitals is a great example. Scan4Safety saves time by knowing where key supplies are, where key pieces of equipment are and where we are in real time. This is not only ensuring efficient use of our funds but also ensures clinicians don’t waste their time and have more time for patients.
Using the taxpayer pound efficiently between us: We will ensure that technology can be shared between us rather than buying it more than once. We are looking to see what we can leverage from each other or simply what can we learn and apply without having to relearn. The Scan4Safety project led by Stuart McMillan at Leeds Teaching Hospitals is a great example. Scan4Safety saves time by knowing where key supplies are, where key pieces of equipment are and where we are in real time. This is not only ensuring efficient use of our funds but also ensures clinicians don’t waste their time and have more time for patients.
Like the use of Alexa in Kirklees, more people will be using technology to help them stay well and independent at home where possible. With more and more technology we need to be careful to also ensure that people feel comfortable with this change. We will aim to make digital as easy as possible for everyone.
Finally, to ensure that we deliver digital advancements in the way people want and need them, we are recruiting Digital Champions. If you are interested in helping shape what we do please contact us at @WYHDigital.
Enjoy your weekend, and don’t spend too much time in front of your computer screen.
Cindy
What else has been happening this week?
West Yorkshire and Harrogate Cancer Alliance
Patient focus at launch of cancer improvement collaborative
 A new way of working together, breaking down organisational barriers and taking a whole- system approach to enhancing patient experience through improving cancer waiting time performance, has been launched in West Yorkshire and Harrogate.
A new way of working together, breaking down organisational barriers and taking a whole- system approach to enhancing patient experience through improving cancer waiting time performance, has been launched in West Yorkshire and Harrogate.
Led by the Chief Executives of our six acute hospital Trusts, the launch of the WYH Cancer Alliance improvement collaborative was attended by more than 100 patients, clinicians, managers and cancer team members from across local places.
The initial focus was on lung and prostate – currently the most challenging pathways – but the plan is ultimately to roll out to all tumour pathways.
 To kick off the launch, the Chief Executives Julian Hartley (Leeds); Owen Williams (Calderdale and Huddersfield); Steve Russell (Harrogate); Brendan Brown (Airedale) and John Holden (Bradford) each gave their personal perspective on why the new approach was important. Martin Barkley, Chief Executive of Mid Yorkshire Hospitals, joined the event later.
To kick off the launch, the Chief Executives Julian Hartley (Leeds); Owen Williams (Calderdale and Huddersfield); Steve Russell (Harrogate); Brendan Brown (Airedale) and John Holden (Bradford) each gave their personal perspective on why the new approach was important. Martin Barkley, Chief Executive of Mid Yorkshire Hospitals, joined the event later.
“For me, it’s about eradicating the ‘what if’ moments – moments at the end of an individual’s treatment where we ask ‘what if we had done things differently,” said Owen Williams.
Steve Russell said there was both a moral imperative’ as one single NHS and a people imperative and responsibility to our patients to break down organisational barriers and focus on the right thing for the individual.”
Brendan then hosted an ‘in conversation’ session with Richard Seddon, a prostate cancer patient, and Sara Williamson, a breast cancer patient who is also Chair of the Yorkshire Cancer Community – formerly the Yorkshire Cancer Patient Forum.
Richard and Sara were invited to share their experiences – both positive and not-so-positive – at the start of the session. This then reinforced from the outset that the event’s focus was on collaboration for patient benefit, and not meeting performance targets just for their own sake.
Both Richard and Sara are now working with the Chief Executives to identify how their experiences can be used by cancer teams in the individual Trusts to improve pathways.
 Four other members of the Cancer Alliance community/patient panel also participated in the event and will continue to co-produce the work of the improvement collaborative over the coming months.
Four other members of the Cancer Alliance community/patient panel also participated in the event and will continue to co-produce the work of the improvement collaborative over the coming months.
They joined table discussions which brought together the stakeholder perspectives from each place, working in locality groups, to identify a range of positive ideas for improvement that could be put into action. A representative from each group then spoke on behalf of their peers to ‘pitch’ their idea to the room.
Sandra Shannon, Chief Operating Officer, Bradford Teaching Hospitals; Bill Cross, Consultant Urologist, Leeds Teaching Hospitals, and Helen Barker, Chief Operating Officer, Calderdale and Huddersfield, shared how their own organisations have approached their improvement journey.
Delegates had been asked to complete postcards in advance of the session, describing both a successful improvement or change they had made, and a change or attempted improvement that wasn’t working.
These were then used to inform ‘pod’ discussions around key themes and the personal pledge that each person attending was asked to post before leaving the event.
All the work undertaken on the day is now being collated and analysed and a work plan being put together to determine the next steps for action. This will be supported by an offer of funding for practical improvement facilitation to each local place, as part of the Cancer Alliance 2019/2020 delivery plan.
“Now the hard work really begins,” said Professor Sean Duffy, Clinical Lead for the Cancer Alliance. “There was a real and buzz in the room, and everyone came with an appetite to make a real difference for patients.
“The powerful lived-experience of Richard, Sara and other patient panel members who are working with us continues to energise our work still further as we move into the action phase. Watch this space!”
Filming of the event and video clips will be available shortly on the Cancer Alliance website and on social media.
Most-At-Risk residents in South Kirkby, Wakefield, reap the benefits of first West Yorkshire and Harrogate lung health checks
Residents most at risk of lung disease in the South Kirkby and Hemsworth areas of Wakefield are reaping the benefits of a pioneering lung health check programme being run from their local GP surgeries.
Around 100 patients attended the Church View Medical Centre on Langthwaite Road in South Kirkby to receive their ‘lung MOT’ during the first week of a targeted lung health check pilot programme led by the West Yorkshire and Harrogate Cancer Alliance, in partnership with Yorkshire Cancer Research. Invitations have been sent to patients of the practice aged 55 – 74 who smoke or used to smoke – individuals who are considered to be most at risk of lung diseases, such as chronic obstructive pulmonary disease and asthma, as well as cancer. Around 95 per cent of all invitations sent out have resulted in patients attending appointments. A number of patients have also taken up the opportunity to access free advice and help to quit smoking which is being provided on site by specialist advisors from Yorkshire Smokefree, with funding from YCR. Evidence has shown that access to such support gives smokers the best possible chance of giving up.
The Wakefield project is part of the Cancer Alliance Tackling Lung Cancer programme, which also includes a similar project in Bradford and also a project in North Kirklees, the selected West Yorkshire and Harrogate site for the national roll-out of targeted lung health checks. Click here to access the full press release.
Bursary scheme promotes early cancer diagnosis – second round of awards announced for West Yorkshire and Harrogate
The second round of a £150,000 scheme to support the early diagnosis of suspected cancers through improvements in patient care and the development of diagnostic staff and has been launched by Yorkshire Cancer Research and the West Yorkshire and Harrogate Cancer Alliance. The two organisations have joined forces on a bursary scheme for radiographers and clinical endoscopists, either qualified or in training. The scheme is offering a total of 30 applicants – 15 radiographers and the same number of endoscopists – up to a maximum of £5,000 each – to encourage excellence and innovation in diagnostic practice.
The 2019 bursary scheme forms part of the Cancer Alliance’s wider New Models of Care programme, which has been designed to deliver systems which speed up the diagnosis of cancer, increase the number of cancers diagnosed at an earlier stage and improve survival. Funding for this two-year scheme has been secured by the Alliance from the national Cancer Transformation Fund. The bursary supports the ambitions set out in the recently- published NHS Long Term Plan, which include an increase in the proportion of total cancers diagnosed at stages 1 or 2 to 75 per cent by 2028, potentially saving up to 55,000 more lives each year.
Closing date is Wednesday 31 July 2019. Further information about the bursary and how to apply can be found on the Cancer Alliance website. From the original £150,000 funding pot, a total of £95,000 remains available to applicants in round two. Click here to access the full press release.
Innovation and Improvement Reference Group
The Innovation and Improvement Reference Group met last Friday. The meeting was chaired by Martin Barkley, CEO for Mid Yorkshire Trust Hospitals, and includes colleagues from WYAAT (hospitals working together), improving planned care, digital, Yorkshire and Humber Academic Health Science Network, NHS England, and the Leeds Academic Health Partnership. Colleagues discussed the benefit from new innovations such as Endocuff (a new type of ‘bowel scope’ that improves colorectal examination for people undergoing bowel cancer tests) and 'Connect to Pharmacy' and how we are making the most of these innovations and other future opportunities.
We made system wide commitments to the adoption of innovation in 2018/19 and some of the achievements were discussed at the programme board. This included our ambitions to spread 21 innovations, including preventing cerebral palsy in preterm labour (PReCePT). We met or exceeded these ambitions for 18 of those innovations including Faecal Calprotectin (a substance that is released into the intestines in excess when there is any inflammation there. Its presence can mean a person has an inflammatory bowel disease such as Crohn’s disease or ulcerative colitis); and six of them we exceeded our ambition for adoption 12 months earlier than expected. This included PINCER (medicines optimisation project) and Urolift (treatment for enlarged prostate).
Based upon this success we will accelerate our adoption of innovation over this year.
Our Partnership has demonstrated how open we are to innovation and how the whole system can work together to the benefit of the 2.6million people living across West Yorkshire and Harrogate.
Board members agreed a new work programme in improvement, innovation and transformation, to be delivered in partnership with Yorkshire and Humber Academic Health Science Network. This programme will build system-wide capability to make the best use of quality improvement and innovation and will exemplify our enthusiasm for improved care within the priority areas of personalised care, primary care networks, Yorkshire Ambulance Service, mental health and outpatients. We’ll keep you posted as the work develops.
Improving Planned Care and Reducing Variation Programme Board
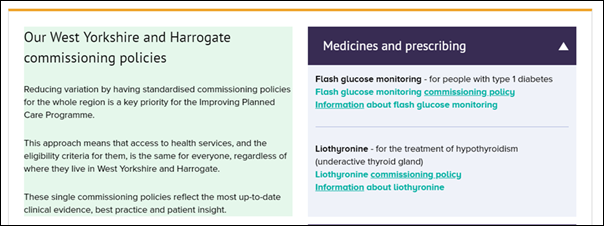
Reducing variation by having standardised commissioning policies for the whole region is a key priority for the Improving Planned Care Programme. This approach means that access to health services, and the eligibility criteria for them, is the same for everyone, regardless of where they live in West Yorkshire and Harrogate.
The approved West Yorkshire and Harrogate commissioning policies for liothyronine (for underactive thyroid) and for flash glucose monitoring (for some people with type 1 diabetes) are now available to access from the Improving Planned Care section on the Partnership’s website here, along with information about each that you may find useful.
Further single commissioning policies for other medications, treatments, musculoskeletal (MSK) services and ophthalmology (eye and vision care) services are being developed through the Improving Planned Care Programme. As with the policies for liothyronine and flash glucose monitoring, these also reflect the most up-to-date clinical evidence, guidance, best practice and patient insight.
Once approved by the Partnership’s Joint Committee, these policies will also be added to the Partnership’s website to create a comprehensive library of single commissioning policies for implementation by all our CCGs. This clearly demonstrates our commitment to ending the so called ‘postcode lottery’ in West Yorkshire and Harrogate.
West Yorkshire and Harrogate Roundtable with Dominic Hardy
 Dominic Hardy visited partners in West Yorkshire and Harrogate on Tuesday. Dominic is the Director of Primary Care and System Transformation in NHS England, leading the implementation of the NHS Long Term Plan’s commitment to create Integrated Care Systems across the country.
Dominic Hardy visited partners in West Yorkshire and Harrogate on Tuesday. Dominic is the Director of Primary Care and System Transformation in NHS England, leading the implementation of the NHS Long Term Plan’s commitment to create Integrated Care Systems across the country.
Dominic met Rob Webster, CEO, South West Yorkshire NHS Foundation Trust and our CEO Partnership Lead as well as colleagues from NHS England, and priority programme leads, including
Dr Sara Munro, CEO for Leeds and York Partnership NHS Foundation Trust and CEO Lead for West Yorkshire and Harrogate Mental Health, Learning Disabilities and Autism Programme; and Carol McKenna, Chief Officer for North Kirklees Clinical Commissioning Group and Chief Officer for Greater Huddersfield Clinical Commissioning Group and also Partnership Lead for our Primary and Community Care Programme.
Dominic also met Dr Peter Davies, Regional Ambassador for Royal College of GPs and Member of the West Yorkshire and Harrogate Clinical Forum; Louise Wallace, Associate Director for Health Integration, North Yorkshire and York County Council and Karen Benstead, Deputy Director of Community Services, Mid Yorkshire NHS Foundation Trust in the morning. Dominic received an update on the work taking place across West Yorkshire and Harrogate including the development of the primary care networks / communities and the importance of improving people’s wellbeing and partner relationships.
In the afternoon, Dominic visited Wakefield District Housing at Castleford and also community partners at the New Wortley Community Centre in Leeds, including Pip Goff, Third Sector and Community Local Care Partnerships Development Manager; and Rachel Ainscough, Senior Local Care Partnerships Development Manager. Dominic also met Thea Stein CEO for Leeds Community Healthcare NHS Trust, Jim Barwick, CEO for Leeds GP Confederation. Both are members of the Local Care Partnership in Leeds.
Rob explained that the principles of our Partnership i.e. the majority of our work takes place in our six local places (Bradford District and Craven; Calderdale, Harrogate, Kirklees, Leeds and Wakefield) in communities and neighbourhoods by local partnerships. Dominic was keen to hear our views on our approach to collaboration in order to deliver the ambitions of our Partnership. With this in mind, sustainability, workforce and financial pressures were discussed including the interface on the front line, for example GPs, and providing seamless care, and streamlining self-referral processes.
Local place based planners (Bradford District and Craven; Calderdale, Harrogate, Kirklees, Leeds and Wakefield)
Local place based planners met on Tuesday. This included an update on the Healthwatch engagement report and the development of our Five Year Plan. Colleagues gave an update on work taking place.
Bradford Teaching Hospitals has recently recruited a new CEO, Mel Pickup who will work with Bradford health care leaders to deliver their local partnership ambitions. The local health care plan is being refreshed to take into account the NHS Long Term Plan and other area priorities.
Kirklees are working through the NHS Long Term Plan Implementation Guidance and are developing a framework / timeline to initiate the work. This approach will be shared with colleagues at the meeting in case helpful.
Harrogate colleagues are looking at opportunities to work together as one clinical commissioning group instead of three from the 1 April 2020. The decision was taken during a meeting in public of the Governing Bodies which represent NHS Hambleton, Richmondshire and Whitby CCG, NHS Harrogate and Rural District CCG and NHS Scarborough and Ryedale CCG, meeting as a ‘Committee in Common’.
A detailed formal proposal will be submitted to NHS England by 30 September. The three CCGs will begin operating as a single, statutory organisation from 1 April next year. They work across three Partnerships like ours (also known as ICSs and STPs).
The Leeds Plan is being refreshed to set out the ambitions of the city. This builds on the local Health and Wellbeing Board aspirations, joint strategic needs assessment and local engagement work, for example findings from the Big Leeds Chat (which will be repeated again this year). Workforce engagement is also very important. They are hoping to publish their refreshed plan in the winter.
Wakefield colleagues are working through the NHS Long Term Implementation Plan in terms of local delivery / operational work. Local partnership conversations are underway. The local health and care plan was refreshed late last year. A number of lunch and learn sessions for Wakefield District colleagues are planned. These will include a focus on our Partnership work.
Colleagues also heard more about the Healthwatch engagement report, the development of our Five Year Plan and the process this would take.
West Yorkshire and Harrogate Organisational Development Programme
Since being formally established as an enabling programme, the System and Leadership Development Programme has been progressing at pace, getting involved in lots of system leadership and Organisational Development (OD) activities with programmes and places, as well as finalising our plans for the next year. We look forward to hearing from each place (Bradford District and Craven; Calderdale, Harrogate, Kirklees, Leeds and Wakefield) about their own programmes funded from the developing leaders resource we secured last year.
Following the Partnership’s annual check and confirm sessions, we have been analysing the OD asks and seeing what interventions we can support, both as collective efforts and bespoke offers. Although we may have been a little ambitious in our plans, with the engagement of the whole OD community, we know we can make a real difference to the ambition of West Yorkshire and Harrogate partnership
One of our priorities is the peer reviews approach and we are confident of securing some resource through the central programme team to enable us to progress with this soon.
We are really excited that recruitment for our talent management role is underway with interviews booked for next Thursday.
We are also leading the process for the Shadow Board this year – thank you to all our partners for providing applications. Shortlisting is underway and nominees will be informed by 19 July if they have secured a place on the 19/20 cohort.
Finally, the West Yorkshire and Harrogate OD Network has become firmly established, with active representation and input from all areas. The network is set up for all with an interest in OD and system leadership, so please come along – it’s not just for those with ‘OD’ in the job title. The next session will be held on 11 September at 9-12 in Kirklees. Please email sherry.

