Collaborating to help people get the best out of their medicines
 My name is Heather, and I am a consultant pharmacist for older people based at the ICB in Leeds as well as working across West Yorkshire. My role is to lead on getting the best out of medicines for older people and includes clinical practice work, leadership, education, and research. I am also the lead for Overprescribing for West Yorkshire.
My name is Heather, and I am a consultant pharmacist for older people based at the ICB in Leeds as well as working across West Yorkshire. My role is to lead on getting the best out of medicines for older people and includes clinical practice work, leadership, education, and research. I am also the lead for Overprescribing for West Yorkshire.
Collaborating with Health Innovation Yorkshire & Humber
Recently key stakeholders across West Yorkshire including the Universities, of Bradford and Leeds, and the West Yorkshire (WY) Overprescribing group and I have been working in partnership with Health Innovation Yorkshire and Humber (formerly known as YHAHSN) to focus on problematic polypharmacy. Problematic polypharmacy is when many medicines are prescribed inappropriately, which can cause side effects, potentially leading to hospitalisation and reduce a person’s quality of life. It is estimated that 10 percent of prescriptions are inappropriate, and in these cases, people could be better served with alternatives to medicines.
Part of our work included a survey across West Yorkshire to capture clinicians’ views on structured medication reviews (SMRs). A SMR is a detailed review of a person’s medicines and their health using shared decision-making conversations and aims to ensure that their medicines are working well for them. The survey showed that:
- People who were having SMRs could be helped to be better prepared for, and participate in, their SMR.
- Pharmacists wanted more training and support around stopping medicines (de-prescribing).
- Clinicians felt that colleagues and the public didn’t always understand the role or importance of SMRs.
The Health Innovation Y&H polypharmacy programme is based on 3 pillars
- Pillar 1 - Population Health Management: Using healthcare data to highlight areas of polypharmacy.
- Pillar 2 - Education and Training: Upskilling the primary care workforce, including GPs and Pharmacists through national Polypharmacy Action Learning Sets. Clinicians can sign up for this free training using the following link Polypharmacy ALS training registration.
- Pillar 3 - Public Behavioural Change: Using ‘Me and My Medicines', a public-facing campaign to change public perception of a “pill for every ill” and encourage people to open up about medicines.
Patient Engagement
Pillar 3 includes rolling out a patient engagement pathway to be used in primary care for SMRs with a focus on shared decision making. The pathway highlights questions people might want to consider asking when having a SMR and aims to empower the person to get the best out of their medicines and to reduce problematic polypharmacy.
The patient engagement material have been co-designed with people with lived experience of polypharmacy and is endorsed by NHS England, Age UK and Professor Tony Avery, the National Clinical Director for Prescribing. The documents are available in multiple languages and forms including easy read and audible versions and are free to download from the Health Innovation website.
Community of Practice
I have also been supporting Health Innovation Y&H with a quarterly Polypharmacy Community of Practice (CoP). CoPs are a group of people who share a concern or a passion and can make improvements by interacting regularly. This proactive approach to share learning and improve practice has involved Academia, Primary and Secondary care practitioners, as well as people with experience of taking many medicines. I have also recently supported a polypharmacy masterclass on the anti-cholinergic burden of medicines’ which was a huge success with over 70 participants from across the county taking part.
I actively encourage healthcare professionals who would like support to reduce problematic polypharmacy/overprescribing within their service to get in touch with either myself or Kirsty Bramley-Dove (Health Innovation Y&H Polypharmacy Clinical Lead); whether it be to understand local data and which patient groups you should prioritise, undertaking training to increase confidence when deprescribing or using the new patient engagement pathway when undertaking a SMR.
Thank you for reading.
Heather Smith (heather.


 More than 6 million lifesaving vaccinations have been given across West Yorkshire, marking another significant milestone in the region’s Covid-19 vaccination programme.
More than 6 million lifesaving vaccinations have been given across West Yorkshire, marking another significant milestone in the region’s Covid-19 vaccination programme.  NHS England’s national director for people, Em Wilkinson-Brice, recently visited Bradford Teaching Hospitals Foundation Trust during NHS England’s People Promise in Action Week earlier in October to see for herself some of the innovative initiatives around staff recognition and flexibility that the Trust are leading on.
NHS England’s national director for people, Em Wilkinson-Brice, recently visited Bradford Teaching Hospitals Foundation Trust during NHS England’s People Promise in Action Week earlier in October to see for herself some of the innovative initiatives around staff recognition and flexibility that the Trust are leading on. Wednesday marked Learning Disability Nursing Day (1 October 2023). This is a national day that celebrates our brilliant Learning Disability Nurses across West Yorkshire.
Wednesday marked Learning Disability Nursing Day (1 October 2023). This is a national day that celebrates our brilliant Learning Disability Nurses across West Yorkshire. This week our NHS West Yorkshire Integrated Care Board Chair, Cathy Elliott, alongside our CEO, Rob Webster, and Yorkshire Ambulance Service NHS Trust, welcomed Cedi Fredrick, Chair of NHS Kent and Medway Integrated Care Board and their CEO Paul Bentley to West Yorkshire.
This week our NHS West Yorkshire Integrated Care Board Chair, Cathy Elliott, alongside our CEO, Rob Webster, and Yorkshire Ambulance Service NHS Trust, welcomed Cedi Fredrick, Chair of NHS Kent and Medway Integrated Care Board and their CEO Paul Bentley to West Yorkshire. The BLOSM ‘Navigator’ pilot at the Calderdale and Huddersfield NHS Foundation Trust has been recognised for its great work at a Nursing Times Awards event. Launched in January 2023, it helps people attending A&E who have experienced trauma and serious violence. The Partnership part funds the service with the West Yorkshire Violence Reduction Partnership. In its first five months, it had supported just under 400 young people. The wider flagship programme delivered across West Yorkshire, has also received national attention for its progress and is the focus of a national policing publication. For more information see the
The BLOSM ‘Navigator’ pilot at the Calderdale and Huddersfield NHS Foundation Trust has been recognised for its great work at a Nursing Times Awards event. Launched in January 2023, it helps people attending A&E who have experienced trauma and serious violence. The Partnership part funds the service with the West Yorkshire Violence Reduction Partnership. In its first five months, it had supported just under 400 young people. The wider flagship programme delivered across West Yorkshire, has also received national attention for its progress and is the focus of a national policing publication. For more information see the  Peter Kyle MP, and Shadow Secretary of State for Science visited Calderdale and Huddersfield NHS Foundation Trust on Monday to see how they are using artificial intelligence (AI) technology in radiology to speed up lung cancer diagnoses.
Peter Kyle MP, and Shadow Secretary of State for Science visited Calderdale and Huddersfield NHS Foundation Trust on Monday to see how they are using artificial intelligence (AI) technology in radiology to speed up lung cancer diagnoses.
 More than 80 colleagues from around West Yorkshire and Harrogate attended a recent education event to raise awareness of Lynch syndrome and to discuss the issues associated with the provision of mainstream testing and improved surveillance. The event was organised by the Optimal Pathways Group team at the Cancer Alliance, including newly-appointed Lynch Syndrome Project Manager/Clinical Nurse Specialist Karen Westaway, together with colleagues from the North East and Yorkshire Genomic Medicine Service. It provided an opportunity for health professionals working in gynaecology and colorectal cancer to collaborate, share best practice and network with colleagues to drive forward an improvement programme for Lynch Syndrome screening and surveillance pathways.
More than 80 colleagues from around West Yorkshire and Harrogate attended a recent education event to raise awareness of Lynch syndrome and to discuss the issues associated with the provision of mainstream testing and improved surveillance. The event was organised by the Optimal Pathways Group team at the Cancer Alliance, including newly-appointed Lynch Syndrome Project Manager/Clinical Nurse Specialist Karen Westaway, together with colleagues from the North East and Yorkshire Genomic Medicine Service. It provided an opportunity for health professionals working in gynaecology and colorectal cancer to collaborate, share best practice and network with colleagues to drive forward an improvement programme for Lynch Syndrome screening and surveillance pathways.
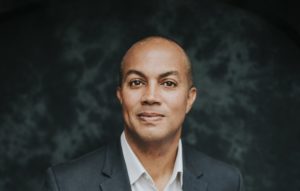 Richard Stubbs, CEO of Health Innovation Yorkshire & Humber, has been appointed as Chair of the national Health Innovation Network. This appointment coincides with the beginning of a new five-year licence agreement for the Health Innovation Network and its 15 regional bodies across England (formerly known as AHSNs) working collaboratively, both nationally and locally, to deliver spread and adoption of innovative technologies and transformational improvements for the benefit of patients, citizens and the NHS.
Richard Stubbs, CEO of Health Innovation Yorkshire & Humber, has been appointed as Chair of the national Health Innovation Network. This appointment coincides with the beginning of a new five-year licence agreement for the Health Innovation Network and its 15 regional bodies across England (formerly known as AHSNs) working collaboratively, both nationally and locally, to deliver spread and adoption of innovative technologies and transformational improvements for the benefit of patients, citizens and the NHS.