Posted on: 12 August 2022
 Hello, my name is Ian and I’m the Director of Strategy and Partnerships for NHS West Yorkshire Integrated Care Board. I wanted to use this blog to talk about the work that we are doing over the coming months to refresh our Partnership’s Five-Year Plan and develop our Joint Forward Plan to deliver it.
Hello, my name is Ian and I’m the Director of Strategy and Partnerships for NHS West Yorkshire Integrated Care Board. I wanted to use this blog to talk about the work that we are doing over the coming months to refresh our Partnership’s Five-Year Plan and develop our Joint Forward Plan to deliver it.
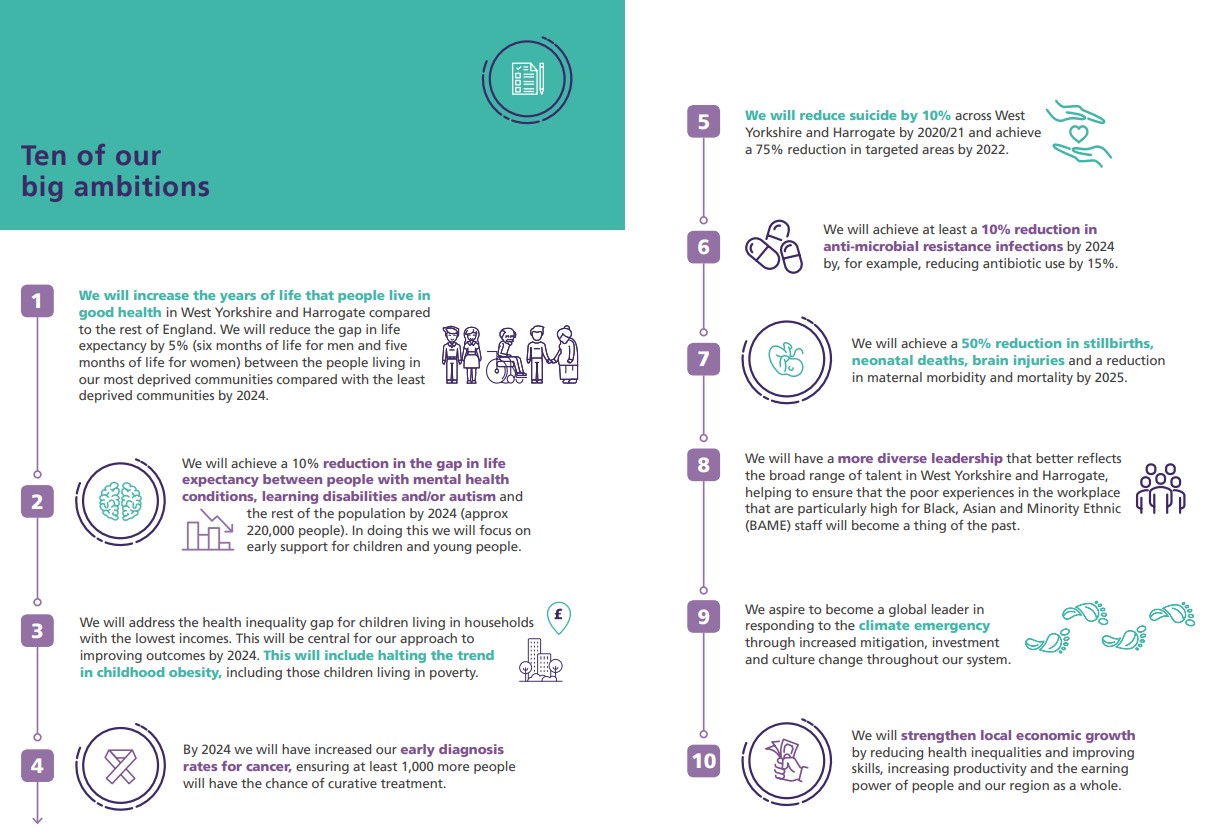
Our first five -year plan was published in March 2020, a matter of days before the first COVID-19 ‘lockdown’. This included our 10 big ambitions setting out what was important to us collectively and reflecting the fact that we are an equal partnership of NHS organisations, local authorities, hospices, Healthwatch communities and the voluntary community social enterprise sector.
Our first three ambitions all relate to narrowing health inequalities across West Yorkshire – for the 10% of people who live in our poorest areas, for people with serious mental illness, learning disabilities and autism, and for children living in poverty. The next four ambitions all deal with improving access to and quality of services, including for example earlier diagnosis of cancers so that they can be cured, and safe and high-quality maternity services.
The final three ambitions all relate to our contribution to wider social and economic goals for our region, including improving the diversity of our leadership so that we are reflective of the communities we serve; contributing to the response to the climate emergency; and ensuring that the £5bn of healthcare investment in West Yorkshire is used to support inclusive economic growth.
Now that we are in the new statutory arrangements, our Integrated Care Partnership (or Partnership Board as we call it) is responsible for overseeing the development of this refreshed strategy and making sure it reflects the needs of the 2.4 million people living across our area.
The Integrated Care Board is responsible for the development of a joint forward plan that will deliver the NHS components of the strategy. This joint forward plan will also need to reflect the requirements set out in the refreshed NHS Long Term Plan (expected to be published shortly) and the Fuller stocktake.
We have started conversations across the breadth of our Partnership about the approach we should take to this refresh. By far the strongest message we have heard to date is that these big ambitions are still the right ones – and our focus should be on how we use the new statutory arrangements to work together to deliver them. So, the theme of continuity of focus and ambition will be central.
But we also know that the situation that the health and care system is operating in has changed significantly over the past two years. The pandemic, and its immediate aftermath have had a profound impact on people’s lives. It has shone a light on the inequity that exists in the communities across West Yorkshire. It has also led to unprecedented demand for services which has added to problems with accessing services that haven’t been seen for over 15 years.
More recently, the cost-of-living increases, driven by fuel and food prices is increasing the number of people in poverty. This will have a direct impact on people’s ability to access services, and their health and wellbeing. We also recognise the impact that this will have on our workforce, and we need to support them in the best way that we can (you can find out more by reading Kate Sims, Director for People for the ICB leadership message next week).
The Healthwatch organisations in West Yorkshire have provided insight into people and communities concerns and priorities for health services in this context, for example:
- People are understandably concerned with access to planned care and general practice services, but they have also identified the importance of good communication for people who are waiting as well as understanding the alternatives available.
- Digital technology has created greater choices for how people access services, but there is concern that this can lead to greater exclusion from care which can widen inequalities.
- People are increasingly concerned about pressure on staff, and workforce shortages across the health and care system, with social care staffing pressures of particular concern.
- People want physical and mental health and care services to be jointed up – and have commented specifically on the need for better hospital discharge processes and more effective planning for moving from hospital to home and care in the community.
Our new strategy will therefore build on the ambitions we have to date but also reflect this reality. These challenges are significant, but as we have seen over recent years, collaboration between the right partners, on the right footprint on the right issues gives us the best opportunity to address them. We also know that whilst the pandemic brought us many challenges, we developed new ways of working and innovated in response to it. It’s important to learn from this and embed the best of this into our strategy and joint forward plan. Our five place partnerships, bringing together the place based integrated care board teams, local authorities, the voluntary and community sector and providers will continue to lead most of this work – ensuring that population health and inequalities are placed front and centre. Our strategy will continue to reflect the five local Health and Wellbeing Board strategies, and the Joint Forward Plan will be built from place. Our provider collaboratives will work at scale where there is a clear case to do so – for example WYAAT (the West Yorkshire Association of Acute Trusts) will continue to oversee our elective recovery work, having reduced the number of two year waits for a planned procedure by over 90% in the first four months of this financial year. At a West Yorkshire level, we will continue to work with partners such as the West Yorkshire Combined Authority and West Yorkshire police on common goals, such as joint work on the climate change agenda, employment and skills, and violence reduction. Our aim is to develop our strategy and joint forward plan over the autumn and winter, in preparation for the 2023-24 financial year. If you or your organisation would like to have your say as part of this work, please do just get in touch. More information will be on our website very soon.
Have a good weekend,
Ian
What else has been happening this week?
NHS to roll out life-changing glucose monitors to all type 1 diabetes patients
 Patients with type 1 diabetes will now be eligible for life-changing continuous glucose monitors after the health service secured a new cut-price deal. The wearable arm gadget sends information to a mobile app and allows diabetes patients to keep track of their glucose levels at all times without having to scan or take a finger prick test.
Patients with type 1 diabetes will now be eligible for life-changing continuous glucose monitors after the health service secured a new cut-price deal. The wearable arm gadget sends information to a mobile app and allows diabetes patients to keep track of their glucose levels at all times without having to scan or take a finger prick test.
Twin sisters Rochelle and Elise Featherstone (pictured above), who work for our Digital Programme, are both living with type 1 Diabetes. Elise was diagnosed with the condition aged just 5 and Rochelle was diagnosed a year later. The sisters started using continuous monitors in June 2019 and describe their experience of the technology as life-changing, dramatically improving their health as well as reducing the negative connotations associated with diabetes. Read more on NHS news.
New analysis reveals trends in children and young people's mental health care in Leeds
 The Networked Data Lab is a collaborative of advanced analytical teams across the UK. They are working together on shared challenges and promoting the use of analytics to improve health and social care. Thanks to the Leeds Data Model, the NHS in Leeds and Leeds City Council are one of five partners across the country who have successfully bid to take part in the initiative.
The Networked Data Lab is a collaborative of advanced analytical teams across the UK. They are working together on shared challenges and promoting the use of analytics to improve health and social care. Thanks to the Leeds Data Model, the NHS in Leeds and Leeds City Council are one of five partners across the country who have successfully bid to take part in the initiative.
The project will look at how partners can work together to use data to improve health and care in the UK, including addressing COVID-19 and widening health and care inequalities. It will do this by identifying and analysing three data sets over three years.
Across the UK, the number of children and young people experiencing mental health problems is growing especially following the Covid pandemic. Mental health services are expanding, but not fast enough to meet rising needs, leaving many children and young people with limited or no support. Too little is known about who receives support and who might be missing out.
 Networked Data Lab (NDL) teams across England, Scotland and Wales have analysed local, linked data sources to explore trends in mental health presentations across primary, specialist and acute services.
Networked Data Lab (NDL) teams across England, Scotland and Wales have analysed local, linked data sources to explore trends in mental health presentations across primary, specialist and acute services.
Analysis in Leeds highlights three areas for further investigation, nationally and locally:
- Adolescent girls and young women are using mental health services more than boys and young men with around 25% of those aged 17-22 are likely to have mental health disorder.
- There is a stark contrast between areas of different socioeconomic deprivation.
- To inform national policy decisions and local service planning and delivery, the quality of data collection, analysis, and the linkage of datasets across services and sectors need to be improved.
- People are less likely to drop out of services if seen virtually and access to services must be easier.
High-quality data and analysis will play a crucial role in targeting preventative interventions, planning services, and improving children and young people’s mental health. In Leeds we have already started to look at how we can improve the quality of data which was an immediate biproduct of this analysis. The development of integrated care system (ICS) intelligence platforms with fully linked datasets across primary, secondary, mental health, social and community care, will be a major step forward.
Working together to improve breast services
 Data analysis shows the breast diagnostic pathway to be one of the most pressured and challenged pathways over the past three years and as a high-volume pathway, accounts for over 25% of all cancer referrals. It therefore contributes significantly to overall system performance across West Yorkshire and Harrogate. WYH breast services and teams strive to provide optimal clinical pathway for the referral and investigation of breast symptoms which may be cancer.
Data analysis shows the breast diagnostic pathway to be one of the most pressured and challenged pathways over the past three years and as a high-volume pathway, accounts for over 25% of all cancer referrals. It therefore contributes significantly to overall system performance across West Yorkshire and Harrogate. WYH breast services and teams strive to provide optimal clinical pathway for the referral and investigation of breast symptoms which may be cancer.
The Cancer Alliance Board has supported a programme of activity to develop a system wide collaborative sustainable solution for breast services, which would enable the system to work together to deliver a flexible and responsive breast cancer service that meets patients’ needs, delivers timely optimal referral and investigation pathways and is able to plan and respond to increases in demand and capacity constraints as a system.
In addition, the Board has also supported progressing a West Yorkshire and Harrogate system solution to address the more immediate capacity pressures and delays in breast diagnostic services and explore and agree arrangements for mutual support through West Yorkshire Association of Acute Trusts (WYAAT) and in collaboration with Trust Chief Operating Officers and Medical Directors.
Involved in the project are representatives from across West Yorkshire and Harrogate, including the breast Optimal Pathway Group Chair Jay Naik and Vice Chair Emma MacInnes; a commissioning representative; Trust cancer managers; breast radiologists and colleagues from the Cancer Alliance Programme Management Office, with Senior Responsible Officer Joanna Bayton-Smith from the Leeds Cancer Programme. Patient engagement is shaping and influencing the work
Priority areas of work include improving referrals and the diagnostic pathway, including piloting the role of breast pain clinics in the pathway; innovation and evaluating the potential role of the PinPoint test; capacity assessment and pathway mapping, and mutual aid and collaborative work.
Cancer care at St James’ Hospital – ‘a beacon for what the NHS should be’, says Richard as his ‘cancer free’ tweet hits the headlines
 Richard Seddon, member of the Cancer Alliance community/patient panel, shared his experiences of two separate cancer diagnoses – prostate cancer and more recently, head and neck cancer – at the last Cancer Alliance Board meeting.
Richard Seddon, member of the Cancer Alliance community/patient panel, shared his experiences of two separate cancer diagnoses – prostate cancer and more recently, head and neck cancer – at the last Cancer Alliance Board meeting.
Richard described his recent care and treatment for throat cancer on Bexley Wing at Leeds Teaching Hospitals as ‘a beacon for what the NHS should be’ with a service that is ‘totally patient-led’.
He also said the support of other head and neck cancer patients – including Lay Board Member Paul Vose – had been invaluable. Richard described the huge interest that had followed his Twitter post about being told he was cancer-free – around 40,000 likes and thousands of comments. In turn, he had been contacted by the Mirror Online and had been happy to share his story to raise awareness of symptoms and the importance of early diagnosis.
Each Cancer Alliance Board meeting opens with a patient sharing their story and experiences.
Delighted to welcome Navina Evans to the Partnership
 We were delighted to welcome Navina Evans, CEO for Health Education England to the Partnership on Thursday 4 August to share the hard work and commitment of many colleagues on our people plan, celebrating our diversity and our differences, service developments and challenges.
We were delighted to welcome Navina Evans, CEO for Health Education England to the Partnership on Thursday 4 August to share the hard work and commitment of many colleagues on our people plan, celebrating our diversity and our differences, service developments and challenges.
A big thank you to all colleagues involved.
NHS Innovation Collaborative for digital health
 A new podcast exploring the relationship between digital inclusivity and heath and care equality has been released by the national Innovation Collaborative for digital health.
A new podcast exploring the relationship between digital inclusivity and heath and care equality has been released by the national Innovation Collaborative for digital health.
Dr Bola Owolabi, Director of Health Inequalities at NHS England and Roz Davies, Associate Director of Thrive by Design, discuss the needs of seldom heard groups, reflect on key learning, progress, and offer advice for teams working to support people through on digital innovations like technology-enabled remote monitoring.
The national Innovation Collaborative for digital health is a shared learning network of health and care professionals, voluntary sector partners, academics and digital innovators working together to accelerate the use of digital technology in health and care.
Listen to the podcast at https://
NHS England feedback on our involvement framework
Last week our Partnership received formal feedback from NHS England about our Involvement Framework (which is our strategy for working with people and communities). There was some very positive feedback and some areas NHSE feel are good practice to share nationally. There are of course areas where we can improve which we will look at in coming months. Thank you to all colleagues and organisations who helped to co-design the framework along its journey to become the framework it now is, showing our commitment to involving people and communities.
Leeds and York Partnership NHS Foundation Trust Annual Members Meeting 2022
 The Leeds and York Partnership NHS Foundation Trust Annual Members’ Meeting took place recently on Tuesday 26 July. The meeting is an opportunity to bring together the Trust’s members, staff, governors and members of the Board of Directors. It is a fantastic day where members have the opportunity to find out about some of the great work the Trust has been doing over the last 12 months.
The Leeds and York Partnership NHS Foundation Trust Annual Members’ Meeting took place recently on Tuesday 26 July. The meeting is an opportunity to bring together the Trust’s members, staff, governors and members of the Board of Directors. It is a fantastic day where members have the opportunity to find out about some of the great work the Trust has been doing over the last 12 months.
On the day there was the official publication of the Trust’s Annual Report and Accounts 2021/22 along with presentations from Chief Executive Sara Munro, Chief Financial Officer Dawn Hanwell and Lead Governor Les France followed by questions for the panel from attendees.