What do integrated care, a Māori proverb and the Dalai Lama have in common?
 I’m Ashley Moore, Associate Director for Community Health Services for Adults in the NHS West Yorkshire Integrated Care Board, Strategy and Partnerships Directorate. But my role (like many others reading this) is really about integrated care – which is, after all, in the title of both our new statutory West Yorkshire Boards. Joining-up care to meet the physical, mental and social needs of people is an on-going journey, and one I feel proud to be part of within West Yorkshire. There’s extensive learning and evidence on what works well and less well around integration, both formally and in people’s lived experience. Ultimately this often draws to similar conclusions including: a shared vision that has the individual at the centre, effective transitions of care, a collaborative team culture and ability to build effective interpersonal relationships, shared approaches to workforce development, interoperable IT systems, and a supportive financial framework.
I’m Ashley Moore, Associate Director for Community Health Services for Adults in the NHS West Yorkshire Integrated Care Board, Strategy and Partnerships Directorate. But my role (like many others reading this) is really about integrated care – which is, after all, in the title of both our new statutory West Yorkshire Boards. Joining-up care to meet the physical, mental and social needs of people is an on-going journey, and one I feel proud to be part of within West Yorkshire. There’s extensive learning and evidence on what works well and less well around integration, both formally and in people’s lived experience. Ultimately this often draws to similar conclusions including: a shared vision that has the individual at the centre, effective transitions of care, a collaborative team culture and ability to build effective interpersonal relationships, shared approaches to workforce development, interoperable IT systems, and a supportive financial framework.
It was though summarised brilliantly at an event with Wakefield colleagues who were looking at the Canterbury health system in New Zealand. There are many layers to the Canterbury experience of integrated care, but at its heart is a Māori phrase which translates to “it’s all about the people”. To that I would add it’s about people and subsidiarity, working within and as near to local communities as possible, giving people authority to act and enabling everyone to fulfil their potential. Building further on that theme, earlier this year NHS England published a national review led by Dr Claire Fuller from the Surrey Heartlands ICS. At the core of Dr Fuller’s review was a renewed vision for integrated community-based care within local neighbourhoods, expanding upon what was set out in 2019’s Long Term Plan and bringing this up to date. In many ways, the review’s conclusions are ones that would be familiar at least a decade ago, but the depth and breadth of the vision (and key learnings it incorporated since the NHS Long-Term Plan) resonated with me.
The Fuller Report also reflects many of the intentions set out in the original West Yorkshire Partnership Five Year Strategy. Over recent months, I’ve had the privilege of being part of a design group supporting the refresh of the strategy. When the group first met in the spring, I imagined it might quite literally look at building a document, and – through engagement with people across the system – gradually map out and curate the potential chapters and content. It’s been an infinitely more enlightening journey than I could have imagined, in no small part because of the opportunity to work with Myron Rogers, of the maxims fame. Myron shared a very powerful personal real-life story with the design group recently which, with his permission, I will briefly recount here. It tells of a team of international systems leaders who had an audience with Dalai Lama in northern India. The Dalai Lama asked the leaders - “So, what is the source of the suffering we experience in today’s world?”. The answers that came back were as unchanging as they were simple: bad leaders, bad politics, bad systems. After hearing these answers, the Dalai Lama paused and sagely replied: “The suffering we experience in today’s world does not have its origin here. It began 100 or 1000 years ago, when people of basically good intent neglected to notice what was arising between them as they set about doing their good work in the world”. Myron described how those words arose within him like a tsunami. As it did for me when I heard the story, albeit in the very different setting of a conference room in Brighouse. It’s clearly not the only factor, but the Dalai Lama’s insight struck me to consider more deeply why genuinely integrating care, when there has been so much good progress, can often still seem so challenging, with many remaining barriers in the way. But these are challenges which I feel (and were exemplified in the Wakefield conversations on Canterbury) are in our collective gift as a Partnership to continue to work together and resolve, because it’s the right thing to do for our populations and for our workforce.
Connecting strategy, “real change happening in real work” (one of the maxims) and having deep conversations that builds shared meaning and purpose is a fundamental part to this. I spend as much time as I can working closely with colleagues at place. It’s very energising and in turn shapes what I do in a way I hope adds value. As an example, and one that chimes with aspects of the Fuller Report, I’ve been working with colleagues on an evolving shared approach across Calderdale, Kirklees and Wakefield exploring ways to integrate further services in the community for population cohorts who tend to be at higher risk of hospital admissions and/or long lengths of hospital stay. This is a multi-professional and multi-sector endeavour, but far more appropriately described by my colleague Jane Close.
 Hello, I’m Jane Close, Chief Operating Officer for Locala CIC and also the clinical advisor to the NHS West Yorkshire Integrated Care Board on community health services for adults.
Hello, I’m Jane Close, Chief Operating Officer for Locala CIC and also the clinical advisor to the NHS West Yorkshire Integrated Care Board on community health services for adults.
Locala is part of the Kirklees place, which in turn works with two acute trusts – Mid Yorkshire, and Calderdale and Huddersfield. We have a strong history of working together across Calderdale, Kirklees and Wakefield districts, and earlier this year a group of us came together to look at further opportunities to collaborative on integrated care pathways in the community. This happened as we were starting to emerge from the pandemic (with the added benefit of being able to collaborate in person) based around a common ambition to further support people to stay well at home and in the community, reduce unnecessary hospital admissions, and minimise the impact of deconditioning and long hospital stays. This all touches on a very wide range of existing services, so we were interested in how we could line this up further, with insights from community services, social care, primary care and the voluntary sector. It’s not just about joining-up services for the sake of it though, it’s what makes a difference to patient and citizen outcomes, supports people to stay healthy and well, and improves access and health equity.
If we get it right, it will provide a more seamless experience and reduce unwarranted variation, and ultimately can be part of a more proactive population health management approach. We know that (at the moment) a lot of activity can end up concentrating on reactive care when someone is already in crisis, and it’s true that there are gains we can make by joining up further these particular services. However, there is a potentially greater prize in how streamlining and integration of more reactive services then creates space in turn to enable a shift to more preventative models of care, that can help tackle health inequalities, and secure the sustainability of services and teams that work within the community. And although we’ve focussed more specifically at service models and pathways across CKW, recognising the nature of our locally interconnected footprint, we’ve also forged links with colleagues working in similar areas in Bradford and Craven, and in Leeds.
What’s positive is that we are not starting from scratch, we’ve got many examples where teams from acute and community, and community and social care, have worked more closely together during and since the pandemic. We are aiming now to go further and, in a way that mirrors the themes in the Fuller Report, understanding what this means going forward for: integrated urgent care – so our populations receive an optimum response depending on the nature and urgency of their need; intensive community support for those with the most complex needs and at high risk; and personalised continuity of care for those with multiple long-term conditions. These areas are of course not all separate, it’s about how we ‘join the dots’ in a way that’s going to make a positive difference for people and the teams that support them.
As part of the overall work across CKW, in Kirklees we are moving to greater integration within the intermediate care services. We are committed to exploring opportunities including developing a culture of integration at all levels of service planning and provision; mapping joint workforce opportunities and supporting new types of roles that span the care and health spectrum; and through opportunities for greater financial integration with clear and costed models to highlight benefits and outcomes. For this to be realised it’s about ensuring improving lives for service users continues to inform everything we do, rather than starting with structures, and that working together as partners is grounded in shared values and mutually supportive behaviours, and increasingly in a truly system integrated way. It’s an on-going and complex journey, as it was before the pandemic, but the momentum being generating shows that spending time to come together on common issues, and develop shared solutions is not a ‘nice to do’ amongst all the busy daily pressures, it’s key to our success.
With thanks to Myron Rogers for permission to share his account with the Dalai Lama. This is based on “Neglecting to Notice”, © 2005, Myron Rogers.
Thank you for reading and have a good weekend
Ashley and Jane


 Hello, my name is Kim.
Hello, my name is Kim. Hello, my name is David. I welcome this opportunity to write my first blog for the Partnership and introduce myself as I begin my appointment as Chief Pharmacist for NHS West Yorkshire ICB. As many of you will know, the majority of my time is spent as Director of Pharmacy at Bradford Teaching Hospitals NHS Foundation. I am fortunate to have worked in Bradford for over 11 years, working across primary, secondary and community and mental health services. It is a privilege to join you as part of a partnership, working with all pharmacy colleagues across Bradford District and Craven, Calderdale, Kirklees, Leeds, and Wakefield District to deliver medicines optimisation transformation.
Hello, my name is David. I welcome this opportunity to write my first blog for the Partnership and introduce myself as I begin my appointment as Chief Pharmacist for NHS West Yorkshire ICB. As many of you will know, the majority of my time is spent as Director of Pharmacy at Bradford Teaching Hospitals NHS Foundation. I am fortunate to have worked in Bradford for over 11 years, working across primary, secondary and community and mental health services. It is a privilege to join you as part of a partnership, working with all pharmacy colleagues across Bradford District and Craven, Calderdale, Kirklees, Leeds, and Wakefield District to deliver medicines optimisation transformation.
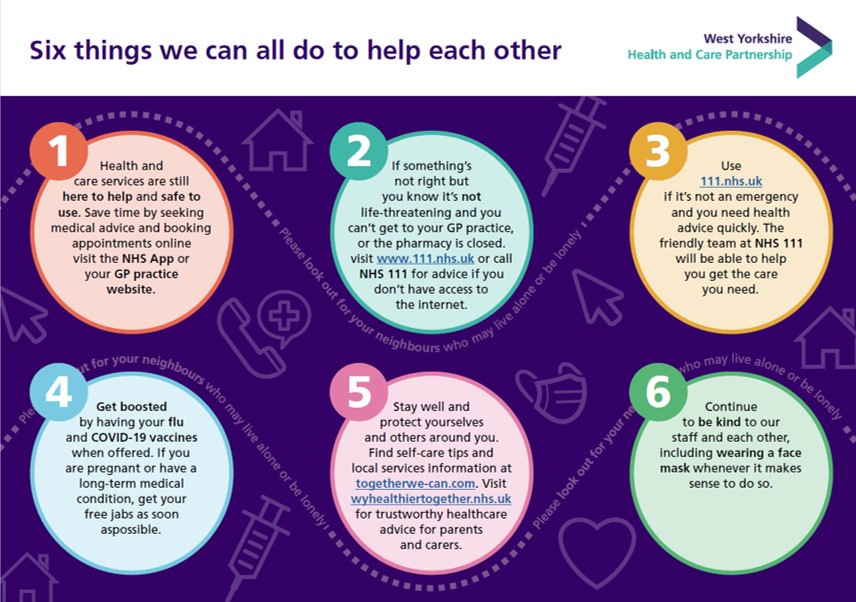
 The Partnership also won HSJ Communications Initiative of the Year for its
The Partnership also won HSJ Communications Initiative of the Year for its  NHS Providers have developed a series of podcasts to include three things needed to drive meaningful change on
NHS Providers have developed a series of podcasts to include three things needed to drive meaningful change on 

 The West Yorkshire Health and Care Partnership People Board met on Friday 11 November. The meeting was Chaired by
The West Yorkshire Health and Care Partnership People Board met on Friday 11 November. The meeting was Chaired by  The final conversation was about the work we are doing to refresh our
The final conversation was about the work we are doing to refresh our  Following an open nomination and interview process we are delighted to confirm the appointment of Dr Richard Vautrey as the Provider Primary Medical Services Partner Member for our
Following an open nomination and interview process we are delighted to confirm the appointment of Dr Richard Vautrey as the Provider Primary Medical Services Partner Member for our 


 The Mental Health, Learning Disability and Autism Partnership Board (the Board) met on 8 November and heard reports from a number of workstreams in the Programme. The Chair, Dr Sara Munro, provided an update on aspects of the programme including the tensions between current operational delivery and transformation ambitions; trying to ensure consistency between systems, regions and national colleagues. The update covered the Quality Agenda, what is being done across system currently to respond to recent high profile quality concerns within inpatient services. Peer review is being built into a proactive West Yorkshire approach.
The Mental Health, Learning Disability and Autism Partnership Board (the Board) met on 8 November and heard reports from a number of workstreams in the Programme. The Chair, Dr Sara Munro, provided an update on aspects of the programme including the tensions between current operational delivery and transformation ambitions; trying to ensure consistency between systems, regions and national colleagues. The update covered the Quality Agenda, what is being done across system currently to respond to recent high profile quality concerns within inpatient services. Peer review is being built into a proactive West Yorkshire approach.