Posted on: 17 July 2020
 Hello, my name is Rachael
Hello, my name is Rachael
I’m really pleased to get to write this week’s blog about shielding and the 112,469 people in West Yorkshire whose front rooms have been their front line in this pandemic.
At the beginning of March, there was awareness that Covid-19 was proving more dangerous for people with existing health conditions and there was a general advisory for about 19 million people aged over 70 or people with a long term condition to take extra precautions. Rapid work was then done by clinical researchers to identify which specific conditions placed people at highest risk, and the people with these conditions became described as the “clinically extremely vulnerable” cohort.
Early modelling indicated that if left unchecked, the virus could have a 15-35% mortality rate for this group of people. This is what prompted the Government to take the unprecedented step to issue advice that the only way to keep safe was to be shielded from catching the virus: this meant that effective immediately they should stay indoors, not go out to work, not go out to shop and not go out to exercise for 12 weeks.
The work to identify who this advice should apply to was in itself an unprecedented use of digital technology. Existing clinical codes do not directly map to the conditions identified. And so expert clinicians were asked to translate the clinical requirements of list into the right subsets of code so that individual people could be identified. In order to get the information out to people as quickly as possible, this then generated a letter or a text sent directly to 2.5 million people, jointly from the Ministry of Health and Social Care and the Ministry for Housing, Communities and Local Government.
Understandably, for most people, to be informed that they were “clinically extremely vulnerable” and too immediately shield at home for the next three months was sobering. Given that the advice was for most people to radically change the way they were living their lives – it’s understandable that there were a lot of different reactions. One friend who is living with a rejected kidney transplant said to me she was relieved that the risk was being taken so seriously. Another who has severe asthma presumed that the text he had been sent was a scam because he didn’t think he could be classed as “vulnerable”.
All of this took place at a rapid speed and without the chance to talk to people about what they would want or need. The Government set up a centralised support offer to deliver essential supplies to people who might need them. Local authorities were tasked with providing all other welfare support and wrap around and primary care was tasked with providing medical advice, support and signposting. And both were being sent separate sets of guidance, written as though we work in isolation.
 In short, as local systems we were starting as far away from integration, personalised care, shared decision making and coproduction as we could be…
In short, as local systems we were starting as far away from integration, personalised care, shared decision making and coproduction as we could be…
And yet – across West Yorkshire, never once did we consider not working together. Never once did we stop trying to put people at the centre of their own shielding experience. And never once did we get lured into thinking that 112,469 people, without previously having had anything in common, were suddenly one homogenous group called “the vulnerable”.
This tendency in the national discourse to describe people advised to shield as “the vulnerable” was problematic for a number of reasons.
Firstly, the way it was being used was that suddenly there just two categories of people: “the vulnerable” and (presumably) “the invulnerable”.
Secondly, it was frequently used in the context to reassure the majority of people that this virus is only really deadly for vulnerable people with “underlying” health conditions. (And yes, I also took exception to people using the term “underlying” as though the conditions people live with every day have just been lurking there with ill intent, waiting for a pandemic to come along to pounce. But, I digress.)
Thirdly, for many people who live with conditions but who are otherwise in good health – they felt it gave the wrong impression. People talked about the feeling of guilt of leaving colleagues to cope without them in workplaces – and they felt that some people were questioning why they should be shielding when they appear physically fit.
Lastly, it confused and conflated being clinically vulnerable to this virus, with other types of vulnerability, such as living with poverty, ill health, with being marginalised or being stigmatised. And so, at a time when reliable and clear advice could actually be, simply put, life-saving - it seemed particularly unhelpful that this term was being loosely applied.
Thankfully however, national headline writers, were not part of the local teams that came together to work out the best ways to offer support and assistance. Each place pulled together a multi-agency team and within a matter of days had begun processing large amounts of incoming data – matching people who were asking for assistance with offers of help and trying in the first instance to ensure that no one was going hungry and no one was putting themselves at risk.
This is really where we can see the value of systems working. In my previous work on community cohesion, I wrote a lot about how relational working engenders trust, and when it reaches a critical mass it is possible to “borrow” trust from one part of the community and introduce it to another. This kind of relational capital is what I saw in spades around this agenda. People from different disciplines coming together for the first time – meeting only in the nether space of conference calls – but the foundations were all them for them to be willing to work together, to overcome all obstacles and throughout have focused their efforts on having the backs of the people doing the hardest part – those holding their own shields.
 And this unswerving person-centred focus has led to loads of great practice, centred on the 4 f’s – of food, pharmacy, finance and friends. On top of the literally thousands of food and prescription deliveries, safe transport to and from hospital appointments as well as other essentials like letters posted and dogs walked; there have been “Breathe Easy” groups learning to zoom; outdoor chair exercise classes in sheltered accommodation; communities of interest leading with expert advice; support workers using their tablets to share messages of support, jokes and songs between service users; virtual coffee mornings; a peer led telephone support service and much, much more.
And this unswerving person-centred focus has led to loads of great practice, centred on the 4 f’s – of food, pharmacy, finance and friends. On top of the literally thousands of food and prescription deliveries, safe transport to and from hospital appointments as well as other essentials like letters posted and dogs walked; there have been “Breathe Easy” groups learning to zoom; outdoor chair exercise classes in sheltered accommodation; communities of interest leading with expert advice; support workers using their tablets to share messages of support, jokes and songs between service users; virtual coffee mornings; a peer led telephone support service and much, much more.
I truly believe this kind of response was only possible because of the culture of partnership working that exists in our local places, as well as the culture of mutual support between places in our Partnership.
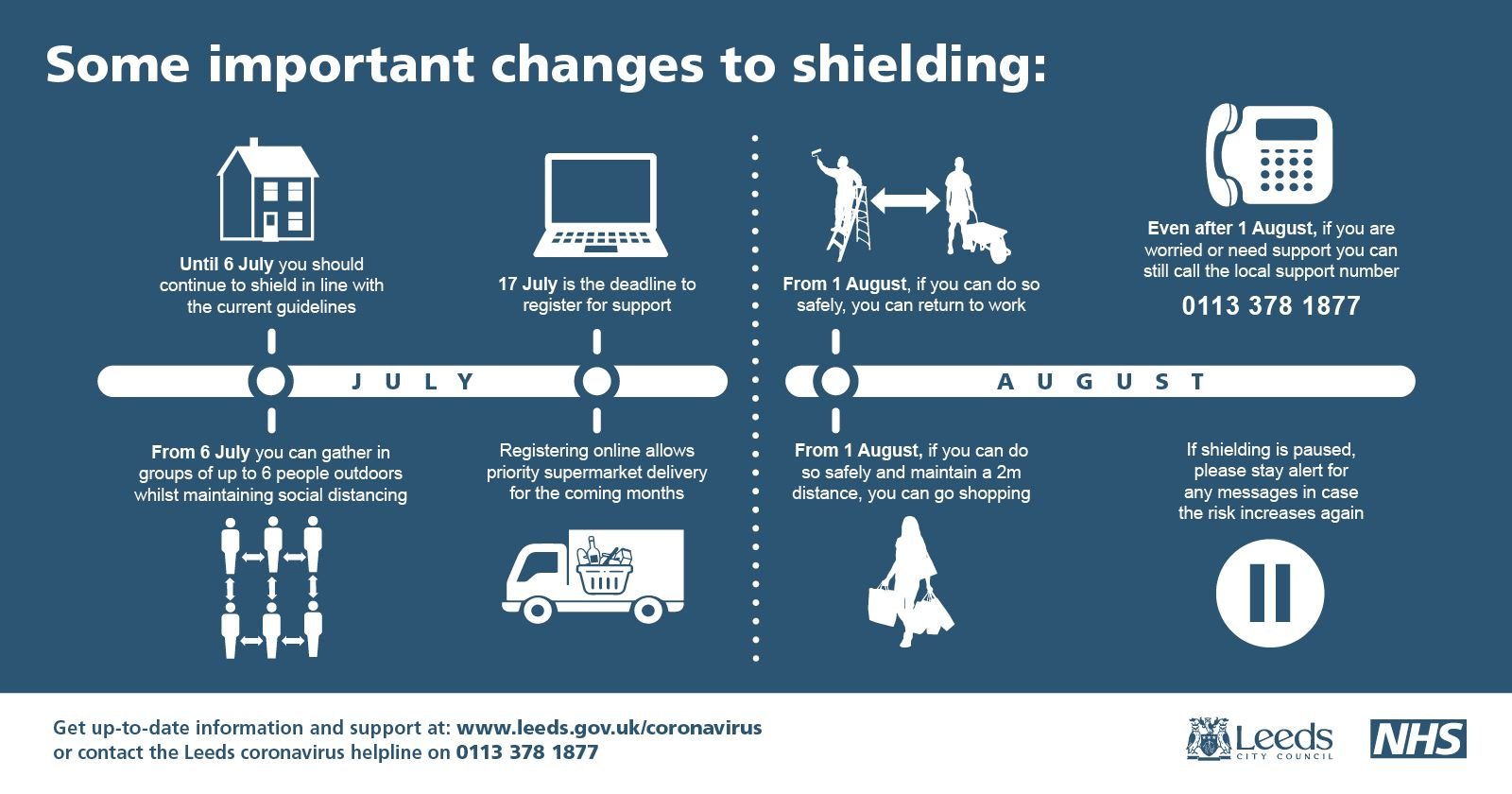
The good news is that as long as prevalence remains low, the Government thinks it might be safe from 1st August for people who are clinically extremely vulnerable to pause shielding at home. Of course we have views and ideas about how best shielding can be managed in future, if there is a need to reintroduce it. And we’re enthusiastically sharing these ideas with our colleagues in central government alongside an excellent insights report done by Healthwatch Leeds and contributed to by 560 people who have been shielding. Read it here.
For most, this pause is being greeted as a welcome relief to return to work, return to the shops and get back to a more normal way of life. But for many, this is also a daunting prospect. They know they remain clinically extremely vulnerable – and many are saying they feel very exposed to the actions of the majority. They want to make the most of the opportunity to see family and friends, to choose their own groceries again – but they need to feel confident that everyone can maintain good physical distance, to maintain handwashing – because if people start to think those rules only apply to “the vulnerable” then we are all more at risk.
For the last 4 months, over 114,000 West Yorkshire residents have carried a heavier burden than most. When shielding is paused on 1st August, we must all be ready to lighten that load a little.
Thanks for reading and have a safe weekend,
Rachael
What else has been happening this week?
Community Resilience Event
Missed the first in a series of our community resilience events? You can watch all our guest speakers presentations here. To those who managed to attend, thank you. We really enjoyed the event and would love to hear your opinion. Please take a couple of minutes to complete our short survey ready for when we plan the next one.
Survey of autistic people's experiences of barriers to urgent, crisis and emergency care launched
West Yorkshire and Harrogate Health and Care Partnership has launched a survey for autistic people to tell us whether they experience barriers to access when trying to use urgent, emergency or crisis care services for a physical or mental health need.
The survey has been created and tested with autistic people so that it is easy to use and yields the highest quality information. The Partnership will use the information gained to develop and improve the way services are delivered to autistic people by a variety of health and care providers across West Yorkshire.
On average, autistic adults in England face significant health inequality, poorer access to healthcare and die 16 years earlier than the general population. However, disability or diagnosis is not the reason for this inequality; instead it is the result of services not meeting people’s needs. For autistic people it can be difficult to stay well and get help when it is needed.
Dr Sara Munro, CEO Lead for West Yorkshire and Harrogate Health and Care Partnership Mental Health, Learning Disabilities and Autism; and CEO for Leeds and York Partnership NHS Foundation Trust said:
“Working with autistic people to ensure that urgent and crisis services are appropriate and easily accessible for neuro-diverse people will help us to identify ways to improve access either by sharing good practice or by testing new ways of working.
At the same time, we are working to make all of our services for neuro-diverse adults, which include people with autism and/or ADHD, more consistent across all of our places in West Yorkshire and Harrogate, so that the approach to assessment and support for physical and mental health needs is the same for everybody, wherever they live.”
West Yorkshire and Harrogate Health and Care Partnership aims to reduce the gap in life expectancy for autistic people, people with learning disabilities and people with mental health conditions by 10% by 2024. Achieving this ambition will make life better for more than 200 000 people living in West Yorkshire and Harrogate.
Update on the Local Maternity System (LMS) co-production and community action project
Due to Covid-19, our important six-month project to reduce inequalities and improve access to care in the LMS had to be paused. That work is now able to start again and will run from July to December. The project is being led by the Local Maternity System and delivered by a team from Magpie Meaningful Marketing, a specialist behaviour change and community engagement agency.
The project aims to:
- Enable women (and their partners and families) to have access to services and information before, during and after pregnancy.
- Understand and respond to how they would like to receive communications, support and care before, during and after pregnancy on a range of issues.
- Understand how to address inequalities and communicate more effectively for those who may be ‘seldom heard’.
We are aiming to gain up-to-date insights, co-create future content, share ideas and strategies and form a community action network made up of women, pregnant women, partners and families with the aim of shaping how we communicate and engage. We will keep you updated as we progress.
The West Yorkshire and Harrogate Organisational Development Network
 The Network brings together organisation development (OD) colleagues from across the Partnership to share and learn from each other. The group met last Friday and reflected that more OD than ever has happened in the last three months with collaboration and delivery through a health and wellbeing lens using online facilitation being key. The group took part in an online masterclass to share and learn insight into this emerging shift of OD thinking and practice. Alongside this, the System and Leadership Development Programme Board discussed three key themes of the last 100 days including; design and launch of the West Yorkshire and Harrogate health and wellbeing offer working with colleagues across Bradford and Craven place; capture of rapid insights and learning from the last 100 days working with Yorkshire & Humber Academic Health Science Network and development of three Black Asian and minority ethnic (BAME) leadership programmes with our BAME network of networks -due to launch in autumn 2020.
The Network brings together organisation development (OD) colleagues from across the Partnership to share and learn from each other. The group met last Friday and reflected that more OD than ever has happened in the last three months with collaboration and delivery through a health and wellbeing lens using online facilitation being key. The group took part in an online masterclass to share and learn insight into this emerging shift of OD thinking and practice. Alongside this, the System and Leadership Development Programme Board discussed three key themes of the last 100 days including; design and launch of the West Yorkshire and Harrogate health and wellbeing offer working with colleagues across Bradford and Craven place; capture of rapid insights and learning from the last 100 days working with Yorkshire & Humber Academic Health Science Network and development of three Black Asian and minority ethnic (BAME) leadership programmes with our BAME network of networks -due to launch in autumn 2020.
There is lots more planned for the future too, including restarting system thinking for our West Yorkshire and Harrogate priority programmes and implementing the learning and innovation gained through rapid insights. Alongside this there will monthly health and wellbeing spotlights, for example with a spotlight on self-care in July.
Developing a suicide reduction campaign
Reducing suicide by 10% across West Yorkshire and Harrogate by 2020/21 and achieving a 75% reduction in targeted areas by 2022 is one of our Partnership’s 10 big ambitions. It is highlighted in the Partnership’s draft Five Year Strategy and the Mental Health, Learning Disability and Autism Five Year Plan. This ambition supports and complements the work taking place in our six local places (Bradford district and Craven; Calderdale, Harrogate, Kirklees, Leeds and Wakefield).
Losing someone to suicide is an experience that no-one should have to go through. It’s important that we work with staff so they are aware of the warning signs, to enable them to support people and to help build resilience – and importantly prevent them taking their life.
By working across the Partnership we can hopefully raise awareness of this subject and most importantly help to save more lives. This is the reason why it is one of our Partnership’s big ambitions. There is a multi-agency Suicide Prevention Advisory Network (SPAN) across all partner agencies. You can read the strategy here. You can also read their Annual Report here.
Our approach also includes working with public health colleagues to create a high-risk decision support tool for primary care and non-mental health services. This will identify people at risk of suicide and will help us target support.
To secure the levels of motivation needed to influence change at pace, we need to think differently about how we communicate at every level, starting with partner staff. We are beginning to develop a suicide reduction campaign, coproduced via a Partnership project team which includes people with experience. It’s important to note we are not starting from scratch. It’s important that we look at successful campaigns elsewhere, and build on the approach taken. The impact of a single approach across our area would potentially be greater than lots of competing campaigns.
Key to all of the above will be working with people with lived experience to ensure the campaign is tailored to meet staff needs. It will be co-produced with representative staff from across the Partnership including BAME colleagues.
The West Yorkshire, Test, Trace, Isolate Programme
 The West Yorkshire, Test, Trace, Isolate Programme met on Friday. It includes colleagues from public health and the NHS. The senior responsible officer for the programme is Martin Barkley, CEO for Mid-Yorkshire Hospitals NHS Trust.
The West Yorkshire, Test, Trace, Isolate Programme met on Friday. It includes colleagues from public health and the NHS. The senior responsible officer for the programme is Martin Barkley, CEO for Mid-Yorkshire Hospitals NHS Trust.
The Association of Directors of Public Health (ADPH), along with other bodies such as PHE UK Chief Environmental Health Officers produced Guiding Principles for Effective Management of COVID-19 at a Local Level. Directors of Public Health are responsible for defining these measures and producing the plans, working through Covid-19 Health Protection Boards.
They are supported by, and work in collaboration with, Gold command emergency planning forums and a public-facing Board led by council members to communicate openly with the public.
Local authorities are working together with NHS Test and Trace and their communities to stop the spread of COVID-19. All councils were asked to extend their existing public health plans into dedicated Local Outbreak Control Plans by the end of June (which they did and have all published on their website), to further strengthen NHS Test and Trace in their area. The work has been supported by £300 million of dedicated council funding.
A new National Local Government Advisory Board has been established to work with NHS Test and Trace to share best practice between communities across the country.
Work to share lessons learned has also been led by a group of 11 local authorities from the breadth of the UK, representing rural and urban areas. Leeds is one of the areas. West Yorkshire Directors of Public Health have been sharing learning and good practice throughout the pandemic (and well before).
West Yorkshire and Harrogate Healthy Hearts continues to make a difference
Cardiovascular disease, also known as CVD, is responsible for one in four premature deaths in the U.K. and it’s one of the biggest causes of death and disability¹.
In West Yorkshire and Harrogate, more than 600,000 people are affected by high blood pressure (hypertension) - a leading cause of heart disease and stroke. We also know that 60,500 people have an irregular heartbeat (atrial fibrillation) and nearly 49,000 people have experienced a stroke or mini-stroke (TIA).²
West Yorkshire and Harrogate Health and Care Partnership is leading an initiative called West Yorkshire and Harrogate Healthy Hearts to tackle cardiovascular disease across the area.
The initiative, delivered in partnership with Yorkshire & Humber Academic Health Science Network is continuing to work with health and care partners including GPs, community pharmacists as well as voluntary organisations and community groups to prevent and care for people with CVD.
Recent data shows an improvement in the management of cholesterol with more than 2,500 patients having a medication review and switching to a stronger statin that can better control their cholesterol. More than 2,000 patients have been identified at risk of cardiovascular disease as their cholesterol is too high and have been offered a statin. This means that nearly 500 patients could avoid a heart attack or stroke in the next 10 years across the area. You can read more here.
Urgent and emergency care (UEC) reset
 Learning from new ways of managing urgent care and avoiding the return of pre-COVID levels of urgent and emergency care activity is a priority. We have to ensure collectively that emergency departments are used only for people who need emergency care. Since the last meeting of the programme board clinical commissioning group accountable officers in Yorkshire and Humber have met and agreed a new approach to the development of an integrated commissioning strategy for Yorkshire and Humber Integrated Urgent Emergency Care Services.
Learning from new ways of managing urgent care and avoiding the return of pre-COVID levels of urgent and emergency care activity is a priority. We have to ensure collectively that emergency departments are used only for people who need emergency care. Since the last meeting of the programme board clinical commissioning group accountable officers in Yorkshire and Humber have met and agreed a new approach to the development of an integrated commissioning strategy for Yorkshire and Humber Integrated Urgent Emergency Care Services.
This will support a set of principles proposed for integrated commissioning; the values and behaviours underpinning integrated commissioning and an operating model for integrated commissioning with agreed outcomes.
There was also support for a single Yorkshire and Humber Strategy, aligned to the national and regional approach to ‘talk before you walk’, for integrated urgent and emergency care with a focus upon:
- Telephone/on line triage via 111/999/General Practice
- Referral to emergency departments/Urgent treatment centres via triage
- Alternative/enhanced pathways via triage/Directory of services
- A pre bookable model A Yorkshire and Humber Task and Finish Group has been established, chaired by Pat Keane, Programme Director of Strategic Projects at Wakefield Clinical Commissioning Group and has included several members of our UEC Programme Board. We have supported work with the Yorkshire Ambulance Service Integrated Urgent Care service to focus on prioritising work on alternative out of hospital services for same day primary care help, such as GP Out Of Hours, extended access schemes and urgent treatment centres; as well as supporting a co-ordinated approach in Yorkshire and Humber to have consistent messages for the public around how to access UEC services. This group has now completed its work and a new Yorkshire and Humber Integrated Urgent and Emergency Care Programme Reset Group is being established. The UEC Programme board will be meeting on 21 July and will continue to focus on integrated urgent care and working collaboratively.
Cancer Support Yorkshire
Charities in West Yorkshire and Harrogate are continuing to flex and adapt to new ways of working to support people affected by cancer during COVID-19. One example is Cancer Support Yorkshire, which has centres in both Bradford and Skipton. CSY, West Yorkshire and Harrogate Cancer Alliance, Bradford Teaching Hospitals and Macmillan Cancer Support work closely on the Next Steps project, which supports those who are reaching the end of their treatment and the project has continue to take new referrals during the lockdown period. Click on the link to read a piece about CSY in the Bradford Telegraph and Argus.
Second wave of Evidence-Based Interventions
The Evidence-Based Interventions (EBI) programme aims to reduce unnecessary medical interventions and prevent avoidable harm to patients by making sure that tests, treatments and procedures routinely available on the NHS are appropriate and clinically effective. In 2018, a public consultation for wave one of the EBI programme received a significant amount of support from patient organisations, commissioners, providers and other representative bodies. It detailed 17 interventions that should no longer be routinely offered on the NHS because they do not work in the vast majority of cases, are only appropriate in certain circumstances or because they have been replaced by safer and less invasive alternatives.
In early 2019, the Partnership agreed to adopt the EBI commissioning policies for all 17 of these interventions. These are now being implemented across West Yorkshire and Harrogate and we are already seeing a significant reduction in the number of inappropriate treatments. The huge impact of Covid-19 has reinforced the importance of the EBI programme. As planned care services are restarted across West Yorkshire and Harrogate, clinicians must be able to focus on effective care for those who need it and not on unnecessary interventions.
Engagement around EBI wave two began on 13 July 2020. The 31 tests, treatments and procedures included in wave two all have little or no clinical effectiveness based on clinical evidence, research and academic studies. There’s more information about the 31 interventions included in wave two on the Partnership’s website here. You’ll also find details about the engagement which is aimed at patients, the public, key stakeholders and other interested parties, as well as providers and commissioners of the interventions.

