The four strategic objectives of our Partnership
Our strategy is centred around our four strategic objectives which set out the core purpose of our integrated care system:
- Reduce health inequalities: for example, if you’re a child or young person living in West Yorkshire, you are more than twice as likely to live in a poorer area than the average England resident.
- Manage unwarranted variations in care: for example, timely identification of deterioration in the health of people with learning disabilities can reduce unnecessary hospital admissions, promote health positively and reduce premature mortality.
- Secure the wider benefits of investing in health and care: for example, NHS investment in supporting local independent social care includes £12million for councils to pay the national living wage to help retain staff.
- Use our collective resources wisely: With around £5bn to invest in people and communities and as the largest group of employers across the area, we’re ideally placed to develop good jobs for good health.
- The Healthy Hearts project in Bradford was scaled up across West Yorkshire so that local places didn’t need to develop their own approach to help reach more people at risk of heart attacks and stroke. This initiative has seen almost 19,000 additional patients added to hypertension register and almost 15,000 additional people treated to ensure their blood pressure is within recommended limits. Another example is that the Academic Health Science Network will launch 10 innovation schemes for cancer, beyond our PinPoint scheme.
Our ambitions for the people of West Yorkshire Improving outcomes in population health and healthcare
We will increase the years of life that people live in good health in West Yorkshire
Health inequalities are avoidable and unjust differences between people or groups due to social, geographical, biological or other factors. These differences have a huge impact, because they result in people who are worse off experiencing poorer health and shorter lives.
 To achieve this ambition, we will take a trauma informed whole systems approach, that addresses the conditions people live in and recognises the importance of the wider determinants on the health and wellbeing of the population.
To achieve this ambition, we will take a trauma informed whole systems approach, that addresses the conditions people live in and recognises the importance of the wider determinants on the health and wellbeing of the population.
This will also require a strong focus on preventing trauma, adversity and ill health by addressing the root causes for health harming behaviours - including tobacco, alcohol, drugs and gambling - in a joined-up systems approach.
A focus on reducing health inequalities for the Partnership will aim to address some of the preventable differences that contribute towards inequalities. Working as a partnership we will consider variations in risk factors for ill health, early diagnosis and screening and access to effective support – all of which contribute towards inequalities in health outcomes.
We will aim for early identification of risk factors and long-term conditions so that we can act early and prevent or delay onset or progression of different health conditions. We will also focus on key areas that contribute most to the years of life lost or lived in ill health, such as cardiovascular and respiratory diseases, cancer and suicide.
We will also learn from national and international policy and research to support our work. For example, embedding the priorities set out in the Women’s health strategy for England.
The work we are undertaking to mitigate the effects of poverty and the cost-of-living crisis will have an impact on quality of life, prevention of ill health and timely access to health and care services.
Access to good quality health and care services continues to be a challenge for the population of West Yorkshire as we recover from the pandemic. Whilst our primary care services continue to provide more appointments than pre-pandemic, we know that public satisfaction with access to services has deteriorated significantly. We continue to work collaboratively to provide timely and appropriate services.
Our hospitals are also working hard to recover from the impact that COVID has had on our diagnostic and elective care services.
We will have increased our early diagnosis rates for cancer
 Our work on enabling the transformation of cancer services in West Yorkshire is coordinated at a system level, via the West Yorkshire and Harrogate Cancer Alliance, which is hosted by the NHS West Yorkshire Integrated Care Board (WY ICB). Cancer alliances are non-statutory bodies, which bring together clinical and managerial leaders from different hospital trusts and other health and social care organisations, to transform the diagnosis, treatment, and care for cancer patients in their local area.
Our work on enabling the transformation of cancer services in West Yorkshire is coordinated at a system level, via the West Yorkshire and Harrogate Cancer Alliance, which is hosted by the NHS West Yorkshire Integrated Care Board (WY ICB). Cancer alliances are non-statutory bodies, which bring together clinical and managerial leaders from different hospital trusts and other health and social care organisations, to transform the diagnosis, treatment, and care for cancer patients in their local area.
Our local cancer alliance has an ambition to bring local partners together to deliver better outcomes and focuses on being empathetic, honest and driven, being people focussed (including a focus on the cancer workforce) and being role models for effective collaboration. They help to oversee the cancer components of the NHS Long-Term Plan and the merger between nationally set priorities for transformation and locally derived need.
They work on a co-production model with patients and service users to ensure that our priorities and ways of working are informed by the experiences of people who are using cancer services. This is critical to ensure that patient experience of care is treated with parity of esteem around what care is delivered.
 The Cancer Alliance works together with colleagues across all our West Yorkshire places, and Harrogate, to ensure that we are taking decisive action across the cancer pathway. This includes improved primary and secondary cancer prevention; better population awareness; promoting earlier diagnosis; achieving better treatment access, including to new therapies and innovations; and adopting a person-centred approach both to follow-up, and end of life care where needed. They also work closely with partners involved in delivering the other ambitions, so that our work is joined up and connected for the common benefit of the people we serve.
The Cancer Alliance works together with colleagues across all our West Yorkshire places, and Harrogate, to ensure that we are taking decisive action across the cancer pathway. This includes improved primary and secondary cancer prevention; better population awareness; promoting earlier diagnosis; achieving better treatment access, including to new therapies and innovations; and adopting a person-centred approach both to follow-up, and end of life care where needed. They also work closely with partners involved in delivering the other ambitions, so that our work is joined up and connected for the common benefit of the people we serve.
We are clear why work to transform cancer care is important. In the future, it is estimated that one in two people could be diagnosed with cancer in their lifetimes, with four out of ten cancers being avoidable if we can achieve changes to lifestyle including healthier weight; safe sun care; reduced tobacco consumption; avoiding alcohol and substance misuse; and acting on wider determinants of health status, including air quality. The burden of cancer is one of the most significant faced by the West Yorkshire ICB and will be across the duration of this and subsequent planning strategies.
Overall, cancer outcomes remain poorer than international comparators, and are strongly associated with wider prevailing health inequalities experienced across West Yorkshire.
Progress against our cancer ambition since 2020 has been good but we know that the data we have is usually around two years in arrears. We know that:
 The total number of patients being referred with suspected cancer into local cancer services is now at pre-COVID-19 (2019) levels. The drop in referrals caused by the pandemic or gap has closed, as people come forward for help with symptoms. Similarly, almost all cancer treatment activity has recovered to pre-pandemic levels
The total number of patients being referred with suspected cancer into local cancer services is now at pre-COVID-19 (2019) levels. The drop in referrals caused by the pandemic or gap has closed, as people come forward for help with symptoms. Similarly, almost all cancer treatment activity has recovered to pre-pandemic levels- The number of patients coming forward and being assessed for cancer symptoms has grown significantly since 2018, as has the number of patients being treated for cancer.
We have also made some good progress with our partners on encouraging uptake of the bowel cancer screening programme through local awareness raising campaigns and the activities of our public health, screening, and primary care network partners. Cancers detected via screening programmes are often at an earlier stage (and are therefore commonly more treatable). West Yorkshire is a leading research centre for new cancer pathways as part of the cancer alliance. This enables us to received grant funding from organisations such as Yorkshire Cancer Research, Macmillan and Cancer Research UK, supporting the development of new treatments and diagnosis of cancer.
We will reduce suicide by 10% across West Yorkshire by focusing on health inequalities, achieving a greater understanding of the impact of inequality on suicide, so that suicide prevention becomes everyone’s business.
 Every death by suicide is devastating and can have a lifelong impact, with each death impacting an estimated 135 people on average. It is our biggest killer of both men under 50 and young people. Suicide is one of our partnership’s wicked issues, with no easy solution that one person or organisation can implement alone.
Every death by suicide is devastating and can have a lifelong impact, with each death impacting an estimated 135 people on average. It is our biggest killer of both men under 50 and young people. Suicide is one of our partnership’s wicked issues, with no easy solution that one person or organisation can implement alone.
Office for National Statistics data shows that despite a focus on prevention in recent years, suicide rates have not reduced. We need to work together to do something differently if we want to change this picture over the next five years. In order to achieve our collective ambition on suicide prevention, all partners have a part to play.
Our vision is to collaborate and create a movement for change - this will make suicide prevention everyone’s business. We have adopted a zero-suicide approach where we believe that even one death by suicide is one too many. We have collaborated on a West Yorkshire suicide prevention strategy, which complements place-based suicide strategies and plans and has 13 core evidence-based themes on which we are focusing our work in the coming years.
We acknowledge that there are national and international factors, some of which are beyond our control, which may impact suicide rates. For example, Government policy, the economic climate and worsening poverty, widening inequalities and discrimination, harmful content online, the gambling industry and its regulation, and the climate crisis each have an impact.
 To mitigate these impacts, we need to:
To mitigate these impacts, we need to:
- Invest in inclusive and preventative measures locally, including becoming a trauma informed system
- Ensure that suicide awareness and suicide prevention is embedded across all organisations as core business
- Eliminating stigma
- Build everyone’s skills and confidence
- Provide inclusive and compassionate support for people with risk factors for suicide and for those affected by suicide.
Errol Murray, founder of voluntary organisation Leeds Dads, said:
“We host a regular text-based chat on our private Facebook group every week. It’s so important people check in with their mates – let them know it’s ok to talk and remember to stay in touch with the people who care about you. For anyone struggling, know there is support out there for you”.
Our Partnership will work together to prioritise suicide prevention, creating a paradigm shift that makes suicide prevention everyone’s business. Every organisation in the Partnership will take demonstrable action on suicide prevention. To support this we have established a suicide prevention website with resources, including links to free training. We also launched the national award winning Check-In staff campaign in 2021, which was followed by the ‘Check-In with your mate’ movement in 2022.
Our Partnership commissioned a film, created by Verd De Gris Arts, which explores mental health and suicide prevention with ex-military personnel. Leaving Service was devised for people working in health, social care, criminal justice – in order to increase awareness of the particular mental health and social situation presented by leaving military service – and the increased suicide risk in this population.
Warning: the film explores suicide attempts, trauma and bereavement.
We will achieve at least a 10% reduction in anti-microbial resistant infections.
We know that the North East and Yorkshire region has the second highest antibiotic rates in England. All parts of West Yorkshire are prescribing over the national target in relation to antibiotic prescribing. Whilst the number of people presenting with infection reduced during the pandemic, data is currently telling us that prescribing is now increasing back towards pre-COVID-19 rates. However, reducing the amount of antibiotics prescribed is only one way we tackle AMR; it is vital that we focus on addressing the prevention and management of infections, thus limiting the need for their use.
 Priorities for our West Yorkshire Anti-Microbial Resistance Board therefore include reducing the number of Urinary Tract Infections across the system and reducing inequalities related to E. coli Gram Negative bloodstream infections.
Priorities for our West Yorkshire Anti-Microbial Resistance Board therefore include reducing the number of Urinary Tract Infections across the system and reducing inequalities related to E. coli Gram Negative bloodstream infections.
Whilst the burden of infectious disease is known to disproportionately impact vulnerable groups, the evidence base for the burden of antibiotic-resistant infections is sparse. However, we do know that rates of prescribing are nationally much higher in highly deprived areas. We are working to understand this in order, to develop actions to change this trend. This work will be set out in our delivery plans.
A priority for our strategy will be expanding successful work in this area across West Yorkshire. The Leeds ‘Seriously’ campaign to raise awareness of antibiotic resistance is a good example of where positive campaigns can have success.
We urge everyone to visit the Seriously website – www.seriouslyresistant.com – to find out what you, your family and friends can do to help tackle antibiotic resistance and to help keep antibiotics working.
We will achieve a 50% reduction in stillbirths, neonatal deaths, brain injuries and a reduction in maternal morbidity and mortality.
 The West Yorkshire Local Maternity and Neonates System (LMNS) covers West Yorkshire and Harrogate and supports a number of Maternity Voices Partnership (MVP) groups across our system to transform our maternity services together. The MVPs are a team of women and their families, commissioners and providers (midwives and doctors) working together to review and contribute to the development of local maternity care.
The West Yorkshire Local Maternity and Neonates System (LMNS) covers West Yorkshire and Harrogate and supports a number of Maternity Voices Partnership (MVP) groups across our system to transform our maternity services together. The MVPs are a team of women and their families, commissioners and providers (midwives and doctors) working together to review and contribute to the development of local maternity care.
Our internationally recognised research programme Born in Bradford aims to find out what keeps families healthy and happy, by tracking the lives of those born in the city. Helping inform a better start in life for our children and young people. This successful programme is now being implemented in other areas of West Yorkshire.
The LMNS has already implemented seven of the initial immediate and essential actions from the Ockenden Report and each hospital trust is currently being measured against these. The remaining issues raised from the report will be considered alongside the Independent Investigation into East Kent Maternity Services report, with a further set of recommendations expected to be published in early 2023. The actions to address these recommendations will form part of the Joint Forward Plan to deliver this strategy.
We know that there are significant ethnic inequalities in maternal and, neonatal healthcare. We will focus on tackling these variations in care, including inequalities in digital access, mental health and workforce.
We continue to work at place and West Yorkshire to address the workforce challenges for maternity and neonatal services. An example of this is the extensive bereavement support offered by Forget Me Not and Martin House Children’s hospices.
 Listening to what people and communities tell us is important. This has been central to the development of all work, including this strategy. As a Partnership we have ongoing conversations with people and communities living in West Yorkshire, supported by Healthwatch partners as set out in our Involvement Framework and the work of our local places.
Listening to what people and communities tell us is important. This has been central to the development of all work, including this strategy. As a Partnership we have ongoing conversations with people and communities living in West Yorkshire, supported by Healthwatch partners as set out in our Involvement Framework and the work of our local places. A number of themes have been raised over the last year (2022) as a result of these discussions in relation to healthcare across West Yorkshire. The changing context has in many cases placed a new emphasis on some of the themes and more recently the cost-of- living crisis has been an escalating issue.
A number of themes have been raised over the last year (2022) as a result of these discussions in relation to healthcare across West Yorkshire. The changing context has in many cases placed a new emphasis on some of the themes and more recently the cost-of- living crisis has been an escalating issue.Of increasing concern is the cost-of-living crisis which continues to escalate and impact on people’s lives. This impacts significantly on their ability to make choices that positively impact their wellbeing, such as accessing healthcare, undertaking activities that support mental wellbeing, eating healthy nutritious food and being able to live in warm, safe housing. These challenges are having a particular impact on those who are living with social disadvantage, serious illness, addictions and those people who are carers.
 There continues to be concern around accessing support for mental health in a timely manner, an issue which has increased with the impact of the pandemic. Of significant concern is access to support for our children and young people and the level of support for children who are waiting for assessment for, or have been diagnosed with, autism. Self-harm rates are rising, and the people we are supporting with mental health issues are becoming more unwell, more quickly than they have previously.
There continues to be concern around accessing support for mental health in a timely manner, an issue which has increased with the impact of the pandemic. Of significant concern is access to support for our children and young people and the level of support for children who are waiting for assessment for, or have been diagnosed with, autism. Self-harm rates are rising, and the people we are supporting with mental health issues are becoming more unwell, more quickly than they have previously.




 To achieve this ambition, we will take a
To achieve this ambition, we will take a  Our work on enabling the transformation of cancer services in West Yorkshire is coordinated at a system level, via the
Our work on enabling the transformation of cancer services in West Yorkshire is coordinated at a system level, via the  Every death by suicide is devastating and can have a lifelong impact, with each death impacting an estimated 135 people on average. It is our biggest killer of both men under 50 and young people. Suicide is one of our partnership’s wicked issues, with no easy solution that one person or organisation can implement alone.
Every death by suicide is devastating and can have a lifelong impact, with each death impacting an estimated 135 people on average. It is our biggest killer of both men under 50 and young people. Suicide is one of our partnership’s wicked issues, with no easy solution that one person or organisation can implement alone. To mitigate these impacts, we need to:
To mitigate these impacts, we need to: Priorities for our West Yorkshire Anti-Microbial Resistance Board therefore include reducing the number of Urinary Tract Infections across the system and reducing inequalities related to E. coli Gram Negative bloodstream infections.
Priorities for our West Yorkshire Anti-Microbial Resistance Board therefore include reducing the number of Urinary Tract Infections across the system and reducing inequalities related to E. coli Gram Negative bloodstream infections.  The West Yorkshire Local Maternity and
The West Yorkshire Local Maternity and  We will achieve a reduction in the gap in life expectancy between people with mental health conditions, learning disabilities and/ or autism and the rest of the population.
We will achieve a reduction in the gap in life expectancy between people with mental health conditions, learning disabilities and/ or autism and the rest of the population. The reasons this gap exists can be divided into two main groups - increased risk of physical health conditions because of different risk factors and medications, and poorer access to health care when it is needed. This is more simply explained by saying that people with SMI, learning disabilities and autism face a range of inequalities that negatively impact their health and lives.
The reasons this gap exists can be divided into two main groups - increased risk of physical health conditions because of different risk factors and medications, and poorer access to health care when it is needed. This is more simply explained by saying that people with SMI, learning disabilities and autism face a range of inequalities that negatively impact their health and lives.
 We will do this by working together to prevent and reduce the causes of trauma and adversity for children, young people and families who are vulnerable and experiencing complex needs, including households living in poverty.
We will do this by working together to prevent and reduce the causes of trauma and adversity for children, young people and families who are vulnerable and experiencing complex needs, including households living in poverty. We see the diversity of all communities and colleagues as a strength to help inform the way we plan, design and commission health and care services for people living across West Yorkshire. We want to make sure that everyone is treated fairly and given an equal chance to access opportunities, ensuring that we meet the needs of everyone so that our population all have good outcomes.
We see the diversity of all communities and colleagues as a strength to help inform the way we plan, design and commission health and care services for people living across West Yorkshire. We want to make sure that everyone is treated fairly and given an equal chance to access opportunities, ensuring that we meet the needs of everyone so that our population all have good outcomes.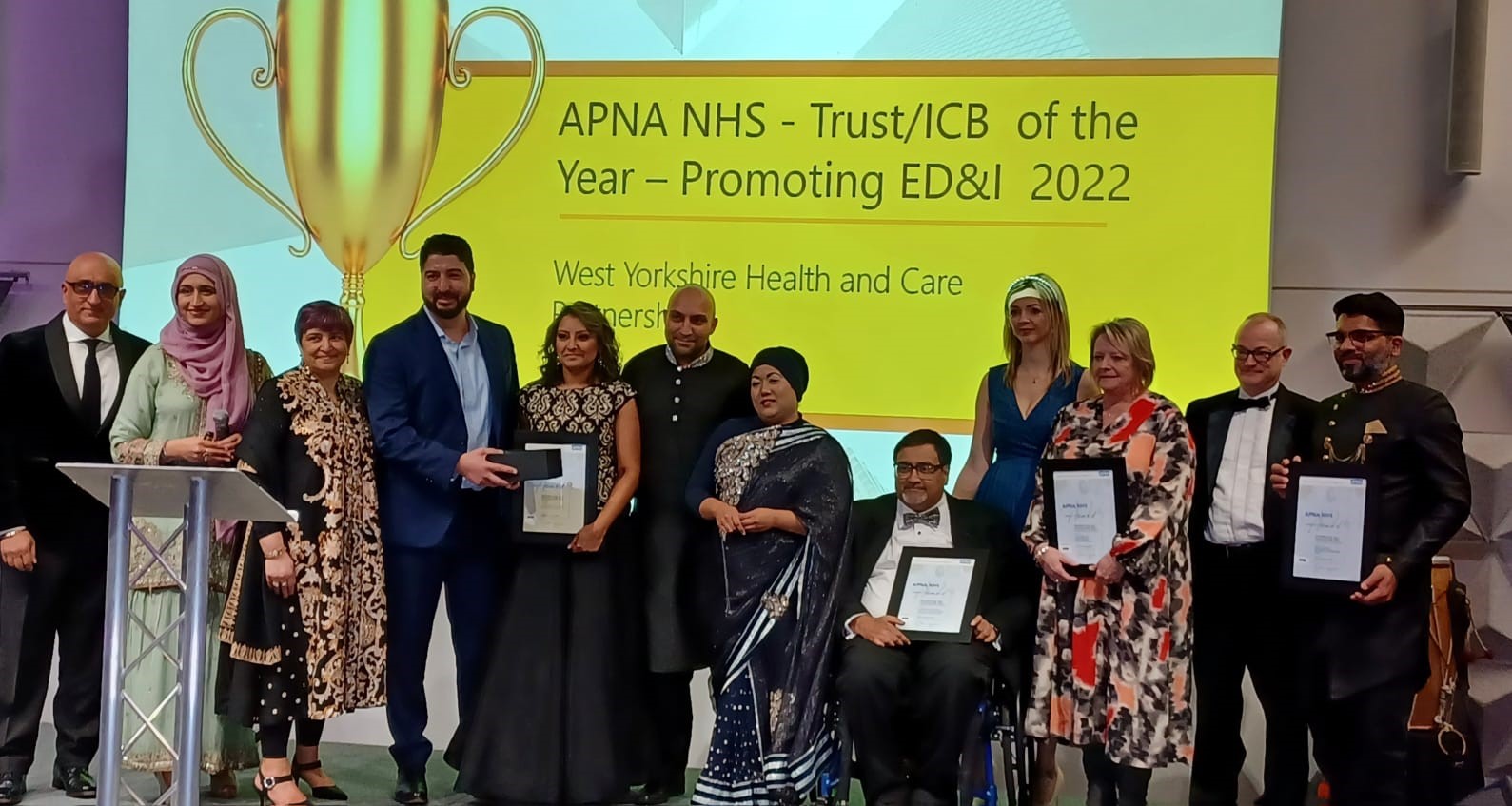
 We know that excess plastics in the environment have a significant impact on our health, as does building antibiotic resistance due to drugs in our watercourses. There are also wide-reaching impacts on physical health, mental health and wellbeing as a result of significant weather events. As a health and care system, we need to also adapt to the impact of climate change now and in the future. This requires a whole system response that includes considerations for supply chains, estates, transports, how we deliver care, housing, planning of the physical environment – so the whole system becomes resilient, which is central to tackling health inequalities and enabling our population, including future generations, to live well.
We know that excess plastics in the environment have a significant impact on our health, as does building antibiotic resistance due to drugs in our watercourses. There are also wide-reaching impacts on physical health, mental health and wellbeing as a result of significant weather events. As a health and care system, we need to also adapt to the impact of climate change now and in the future. This requires a whole system response that includes considerations for supply chains, estates, transports, how we deliver care, housing, planning of the physical environment – so the whole system becomes resilient, which is central to tackling health inequalities and enabling our population, including future generations, to live well. We know that economic activity has a significant impact on health and wellbeing. Having a purpose and a living wage contribute significantly to a sense of belonging and being able to live a life well. Both the pandemic and the cost of living crisis has significantly impacted on this for many people in West Yorkshire.
We know that economic activity has a significant impact on health and wellbeing. Having a purpose and a living wage contribute significantly to a sense of belonging and being able to live a life well. Both the pandemic and the cost of living crisis has significantly impacted on this for many people in West Yorkshire.